(UroToday.com) In a podium presentation in the Renal Cancer I – Localized session at the 19th Meeting of the EAU Section of Oncological Urology, Dr. Porpiglia presented on the role of augmented reality in robotic assisted partial nephrectomy. He began by defining, in this context, augmented reality as the superimposition of 3-dimensional (3D) virtual models over the real anatomy of patients. This approach, using a specifically constructed platform, allows for enrichment of additional information to the real environment which allows for a better understanding of anatomy and disease. Clinically, the most relevant application is for intraoperative navigation.
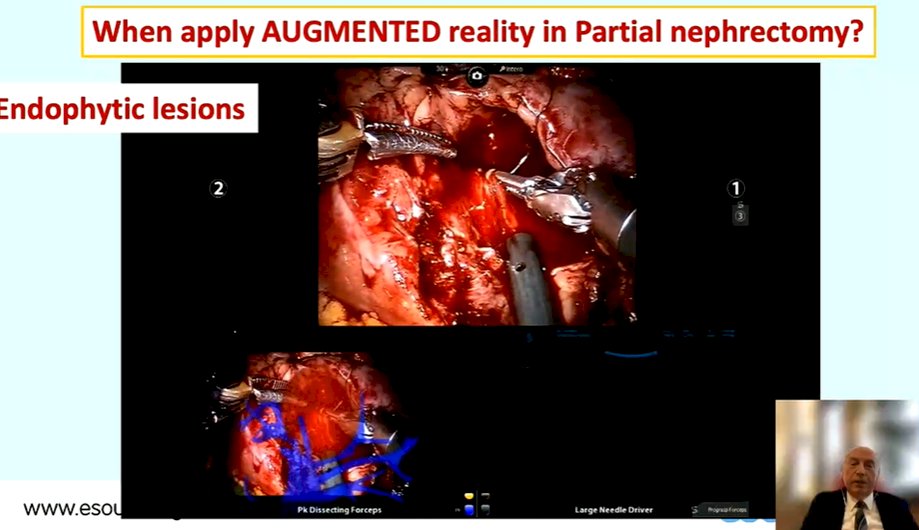
Dr. Porpiglia emphasized that there are two key roles for the use of augmented reality in partial nephrectomy. The first of these relates to its ability to delineate tumor characteristics. This is particularly useful in the case of endophytic lesions which may be difficult to appreciate based solely on the laparoscopic vision. Using a number of intra-operative videos, he highlighted the value of augmented reality and image overlay to allow appreciation of the limits of entirely endophytic tumors in which there is no apparent lesion at the level of the renal capsule to guide operative approach.
Additionally, he emphasized that this approach allows an enucleating tumor resection and can inform selective suturing during renorrhaphy.
Secondly, Dr. Porpiglia highlighted the value of augmented reality to outline the renal vascular anatomy. Better visualizing hidden vessels facilitates selective arterial clamping.

Again utilizing intra-operative to highlight his point, Dr. Porpigilia highlighted that the use of augmented reality allows identification of small renal arterial branches that feed the tumor.
Citing publications from 2018, 2020, and 2021 from his own group, he emphasized that the use of 3D augmented reality informed robotic assisted partial nephrectomy provides a number of key surgical advantages compared to a standard robotic surgical approach. First, as highlighted above, there is better tumor localization which is particularly beneficial for patients with endophytic tumors. Second, the surgical approach can be modified, particularly with respect to management of the renal hilum / pedicle and tumor. Notably, he emphasized that 90% of cases could be performed as they were planned pre-operatively. Third, during the reconstructive phase of the partial nephrectomy during the renorrhaphy with better identification of the intraparenchymal anatomy. For patients, these surgical advantages translate to clinical benefits. First, there is increased utilization of selective clamping, sparing global renal ischemia. Second, there is a higher rate of enucleating resections, with resulting greater sparing of normal renal parenchyma. Taken together, it is therefore not surprising that there were better renal functional outcomes when the augmented reality approach was utilized. Additionally, the use of augmented reality was associated with fewer post-operative, surgery related complications than a traditional surgical approach.
Despite the promise of this approach, Dr. Porpiglia emphasized that there are limitations currently which needed to be overcome to provide widespread clinical utility. First of these, he emphasized the importance of improvements in the precision of the estimation of renal vascular anatomy. Second, he highlighted logistic considerations with respect to automatic overlapping.
In the context of renal vascular anatomy, to date, 3d models have shown an ability to provide accurate pre-operative planning and intraoperative overlay. As a result, this has facilitated higher rates of selective vascular clamping (76% in his center). In approximately 10% of cases, even when selective clamping is planned, global renal ischemia with main branch renal arterial clamping is required.
However, he considered it “a matter of perspective” as to how we approach these data. First, he emphasized that we don’t need to just consider the anatomic direction of the artery towards the tumor when considering proper selective clamping but the areas of tumor growth and the arteries which supply this tissue. Thus, to improve the efficacy of augmented reality, we need to improve the accuracy of 3D model reconstructions to identify renal vascular regions at two levels: parenchymal vascular regions and the deep vasculature. Considering the first of these, Dr. Porpiglia emphasized that we need to integrate both classic anatomic-surgical principles with mathematical models to predict the extent of vascular regions in which the tumor is growing.

Again, he used a number of examples of intra-operative videos to emphasize this value of augmented reality for selective clamping. In a sample of 48 patients, 100% of selective clamping attempts were effective. Further, a comparison of the extent on bidimensional images showed a high level of concordance (kappa = 0.94) between the virtual areas of ischemia and anatomic ischemic areas.
Additionally, considering the question of resection and renorrhaphy, Dr. Porpiglia emphasized that there may be lacerations to deep vessels. More precise delineation of this vascular anatomy is expected to help with the renorrhaphy process and targeted suturing to avoid blood loss.
Second, he emphasized that there is a constant manipulation of the 3D model to adjust the overlapping is currently an impediment to the usability of this approach. It currently requires a dedicated assistant, who has their own learning curve and are limited by human reaction times. However, as demonstrated by work that is currently in press, advances have allowed for camera movement following anchoring of the model. This allows the surgeon to identify and demarcate the lesion margins with constant, real time assistance from the automatic augmented reality. Using of this approach was safe and effective with no intra-operative complications and no positive surgical margins. Dr. Porpiglia suggested that this automatic augmented reality may improve the usability of this approach by shortening the training time necessary, minimizing the learning curve, and reducing costs.
In summary, he emphasized that augmented reality in robotic assisted partial nephrectomy represents the most advanced and complete application of 3D virtual modelling which allows for improved surgical and clinical outcomes.
Presented by: Francesco Porpiglia, Division of Urology, University of Turin, Italy


