(UroToday.com) In a podium presentation in the Renal Cancer I – Localized session at the 19th Meeting of the EAU Section of Oncological Urology, Dr. Giusti presented on advances in conservative treatment approaches in patients with upper tract urothelial carcinoma (UTUC). He began by emphasizing that conservative treatment should be preferred for patients with low-grade disease which radical nephroureterectomy is preferred for patients with high-grade disease or high volumes of disease. While the guidelines recommend kidney sparing surgery for patients with low-risk disease, he emphasized that there are few details provided in the guideline. However, it is emphasized that flexible ureteroscopy should be performed and that complete tumor resection or destruction is necessary.
Dr. Giusti first then considered the question of what ureteroscope should be used. He highlighted that the image quality of a reusable digital ureteroscope is vastly superior, both to conventional optical scopes and to single use digital scopes.

He highlighted that, in addition to the improved optics and visualization that these scopes provide, they offer additional technologies such as narrow band imaging and S technology which may aid in tumor identification. However, he acknowledged that the literature supporting the use of these approaches is relatively limited for upper tract disease. One publication from Dr. Traxer’s group suggested that the use of NBI may improve tumor detection by up to 23%, owing to better visualization of submucosal vasculature. While assessed in bladder cancer, to date, there are no data evaluating S technology in upper tract disease.
Second, he considered further adjuctive technologies that may assist with diagnosis and treatment planning. These include so called “optical biopsy” using imaging such as the use of intraoperative optical coherence tomography. This offers real-time information on histopathologic details such as tumor grade and stage utilizing light reflectivity, in parallel to ultrasonography. Cellvizio, confocal laser endomicroscopy is an alternative technology which seeks to characterize tumor grade.
Dr. Giusti then considered the question of treatment modality. Again, the guidelines are not prescriptive, though most urologists have traditionally used holmium laser due to their familiarity with this approach. However, Dr. Giusti suggested that thulium:YAG may provide better results for this indication as a result of a deeper tissue penetration effect, better coagulation, and more efficient treatment. Additionally, UTUC ablation with thulium:YAG was associated with lower rates of complications than with holmium. While there is less bleeding with use of the thulium:YAG laser (which can improve visualization), this approach generates a lot of necrotic tissue (which may obscure identification of the tumor base and residual disease). Therefore, he suggested an approach combining the two. In doing so, the surgeon would start by using a thulium:YAG laser to ablate the exophytic portion of the tumor and then subsequently use a holmium laser afterwards to remove the necrotic tissue and treat the base and any residual disease.
He highlighted a more recent advance with the use of superpulsed thulium fiber lasers. This fibe provides the higher water absorption, allowing use of higher pulse power. As a result, this should lead to improved cutting and reduced carbonization. In both ex vivo and in vivo studies, this has been shown to translate to a clinically meaningful effect with a resulting good compromise between the excellent hemostasis seen with thulium:YAG lasers and the tissue cutting of the holmium laser with a more tolerable degree of carbonization.
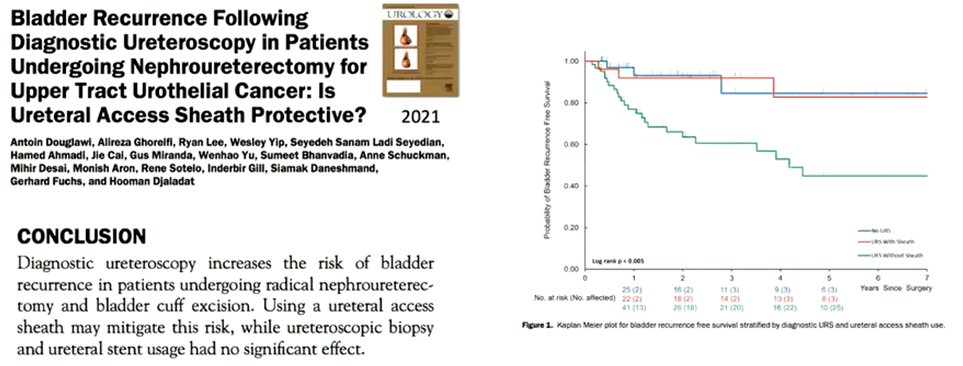
Third, Dr. Giusti considered the question of bladder recurrences. The literature has shown that diagnostic ureteroscopy, ureteroscopic biopsy and ureteroscopic treatment may be associated with intravesical recurrence. This has been supported by systematic reviews and meta-analyses. However, recent data has suggested that use of a ureteral access sheath may attenuate this risk.
The use of intravesical chemoprophylaxis for bladder cancer recurrence after radical nephroureterectomy has been established based on randomized data. While no such data exists following diagnostic or therapeutic ureteroscopy, the EAU guidelines suggest that the rationale is comparable. However, Dr. Giusti emphasized that prospective data are needed in this context.
Fourth, Dr. Giusti considered the question of adjuvant upper tract therapy. To date, based on systematic reviews, the literature is not promising: there is no difference in recurrence rate between treated and untreated individuals. Perhaps not surprisingly then, no differences in type of drug used (mitomycin C vs BCG) or approach used (antegrade vs retrograde) were identified.
However, intraluminal chemotherapy has shown benefit for chemoablation of low-grade tumors using Jelmyto, based on the phase 3 OLYMPUS trial. Dr. Giusti emphasized that this is a promising treatment approach with complete response rates exceeding 50% though, when counseling patients, we need to stress the relatively high risk of ureteral stenosis.
Finally, considering the ongoing monitoring of patients, he emphasized that recently presented data shows that EpiCheck has a higher sensitive and negative predictive value for high-grade disease than urinary cytology.
In closing, Dr. Giusti emphasized that radical nephroureterectomy remains the gold standard for treatment of high-grade disease. Conversely, for those with low-grade disease, kidney sparing surgery should always be offered. Continuous evolution of the technology used for kidney sparing treatments should serve to improve patient outcomes while maintaining safety and reducing the effect on patients’ quality of life.
Presented by: Guido Giusti, Head of European Training Center of Endourology, Ospedale San Raffaele-Turro, Milan, Italy


