At this time, there are 4 reported in the adjuvant setting - ASSURE (Haas NB et al. Lancet 2016), S-TRAC (Ravaud A et al. NEJM 2016), PROTECT trials (Motzer RJ et al. JCO 2017), and ATLAS (Gross-Goupil M et al. Ann Oncol 2018). There are 2 ongoing trials that are likely to report soon – SORCE and EVEREST. He had a summary of these 6 studies and their designs, as seen below:
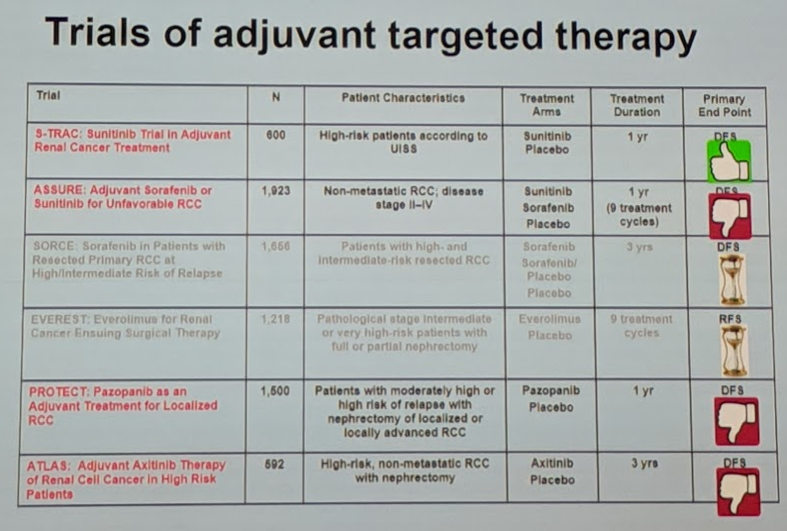
At this time, only S-TRAC has been positive – with an improvement in DFS. He noted the following:
- S-TRAC had the highest risk population – the cleanest dataset.
- S-TRAC also had the least dose reduction and dose modification – patients stayed on the initial recommended dose
- SORCE is likely reported next year – extended to 3-year follow-up when they saw the 1-year results of ASSURE
He also pointed out that many of these studies have not been able to report on overall survival – but many point to slowly splitting K-M curves on immature data as a possible signal of OS benefit. However, he cautions that this is more likely an artifact of the low number of patients alive (and at risk) in these populations at the later part of the KM curves. He does not believe any OS benefit would be meaningful.
He again reiterated the common question in the discussion of adjuvant therapy for RCC – are we targeting the right targets and endpoints?
- All the current agents being assessed target the angiogenesis pathways – which makes sense for patients with metastatic RCC and active angiogenesis pathways, large vascular supply. However, for micrometastatic disease, this has less biologic rationale.
- Is disease-free survival an appropriate endpoint for adjuvant therapy discussions and for RCC? Is it a true surrogate for overall survival?
- Is it just prolonging time to symptomatic progression but not changing overall survival?
- Surveillance of metastatic RCC – a recent phase II study by Heng et al. (Lancet Oncology 2016) demonstrated that patients with favorable and intermediate mRCC actually take 14.9 months to progress to needing targeted therapy. Surveillance for these patients is a reasonable option. So perhaps immediately starting patients on systemic therapy after a nephrectomy isn’t warranted, especially as there is no clear overall survival benefit.
- Indeed, when looking at the placebo arms of the RCTs listed above, 40-60% of patients remained disease-free at 4-8 years after nephrectomy – suggesting that overtreatment with adjuvant therapy would be significant.
- NNT using ASSURE: 136 patients would need to be treated for 1 patient to derive benefit
- NNT using S-TRAC: even with S-TRAC, 9 patients would need to be treated for 1 patient to derive DFS benefit, not even OS benefit
- Toxicity – as many patients would need to be treated to derive some benefit, toxicity profiles become important. Unfortunately, as a class, targeted therapies have significant toxicity profiles.
- Grade 3-4 adverse events in these studies were not negligible
- More importantly, dose reduction or drug discontinuation was common amongst all the RCTs – mostly due to side effects
- Dose likely matters
- In a pooled analysis of the PROTECT study data by Maxine Sun et al. (EU 2018), they noted that while risk category didn’t seem to impact outcomes, patients who received full-dose treatment appeared to derive some benefit compared to those not receiving full-dose
- S-TRAC, the only study to show benefit, is the only one of the first 3 studies to have patients start and maintained on full-dose sunitinib – and may be one reason it was positive, while the others were negative
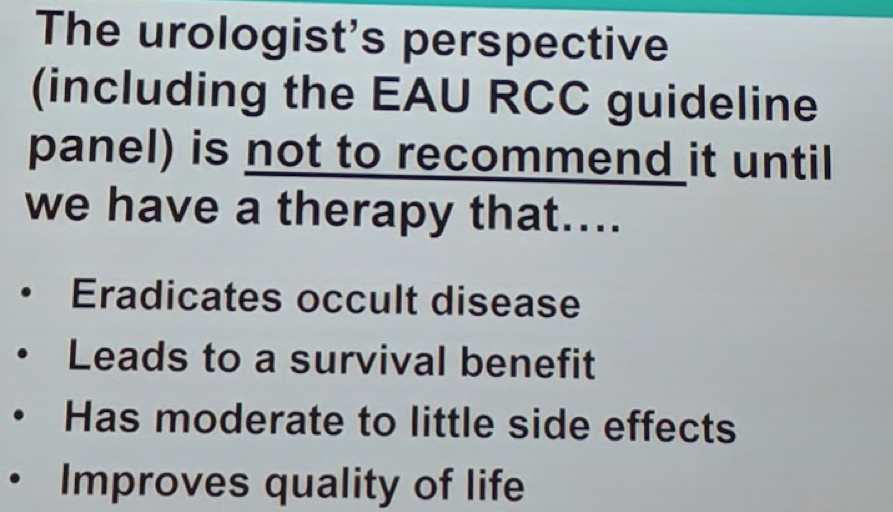
This is where the potential promise of immunotherapy lies, as it appears to be much better tolerated than targeted therapies.
Presented by: Axel Bex, MD, Ph.D., Netherlands Cancer Institute, Department of Urology, Amsterdam, Netherlands
Written by: Thenappan Chandrasekar, MD. Clinical Instructor, Thomas Jefferson University, Twitter: @tchandra_uromd, @TjuUrology, at the 16th Meeting of the European Section of Oncological Urology, #ESOU19, January 18-20, 2019, Prague, Czech Republic
Further Related Content:
Adjuvant Therapy after Nephrectomy for High-Risk Renal Cell Carcinoma: The Oncologist's Perspective


