(UroToday.com) The 2023 European Society of Medical Oncology (ESMO) Annual Congress held in Madrid, Spain between October 20th and 24th, 2023 was host to a prostate cancer abstracts poster session. Dr. Craig Jones presented linked healthcare systems data from the STAMPEDE Arm H trial evaluating the impact of prostate radiotherapy on long-term obstructive uropathy rates in patients with metastatic hormone sensitive prostate cancer (mHSPC).
STAMPEDE (Arm H) was an open label, randomized controlled phase III trial of 2,061 men at 117 hospitals across Switzerland and the UK. This arm randomized patients with de novo mHSPC in a 1:1 fashion to standard of care with or without radiotherapy between January 2013 and September 2016. Standard of care was lifelong androgen suppression with upfront docetaxel permitted from December 2015 onwards (18% of total cohort). Men allocated radiotherapy received either a daily (55 Gy in 20 fractions over 4 weeks) or weekly (36 Gy in six fractions over 6 weeks) schedule that was nominated before randomization.
At a median follow up of 37 months, overall survival benefits were only seen in the low volume group (HR: 0.68, 95% CI: 0.52 - 0.90) with restricted mean survival time improved by 3.6 months from 45.4 to 49.1.1 Updated results of this trial published in 2022 at a median follow up of 61.3 months, continued to demonstrate overall survival benefits for prostate radiotherapy in patients with low metastatic burden (HR: 0.64, 95% CI: 0.52 - 0.79, p < 0.001), whereas no benefit was seen in patients with a high metastatic burden (HR: 1.11, 95% CI: 0.96 - 1.28, p = 0.164; interaction p = 0.001).2
Recent data from PEACE-1 presented at ASCO 2023 demonstrated that the addition of prostate radiotherapy to standard of care (+/- abiraterone acetate) was associated with significant improvements in the time to serious genitourinary events in the overall cohort. This is likely due to men with advanced prostate cancer experiencing local progression that may lead to an increased subsequent risk for upper urinary tract obstruction/deterioration. As such, the objective of this study was to evaluate the impact of prostate radiotherapy on the time to upper urinary tract obstruction using accessible, high quality healthcare systems data that is able to provide accurate event data beyond standard trial follow-up (STAMPEDE Arm H).
In this study, the authors used linked healthcare systems data from Hospital Episode Statistics (HES) with follow-up to March 2021. This analysis included England-based patients who were randomized to Arm A (standard of care) and H (standard of care + radiotherapy). Radiotherapy was delivered either daily (55 Gy in 20 fractions over 4 weeks) or weekly (36 Gy in six fractions over 6 weeks). Interventions for upper urinary tract obstruction (including percutaneous nephrostomy and or ureteric stent insertion) were identified using a comprehensive coding framework using International Classification of Diseases (ICD 10) diagnosis and Classification of Interventions and Procedures (OPCS 4) codes.
Multivariate flexible parametric survival models adjusted for randomisation stratification factors were used to estimate the treatment effect of primary radiotherapy on the cumulative incidence of upper urinary tract obstruction and the sub distribution hazard ratios.
Of the 2,061 patients in the trial, 1,791 (88%) were followed up by English-based hospitals and connected healthcare systems data were available for 96% of such patients. Nineteen patients who had an upper urinary tract obstruction-related intervention in the 90 days prior to randomization were excluded.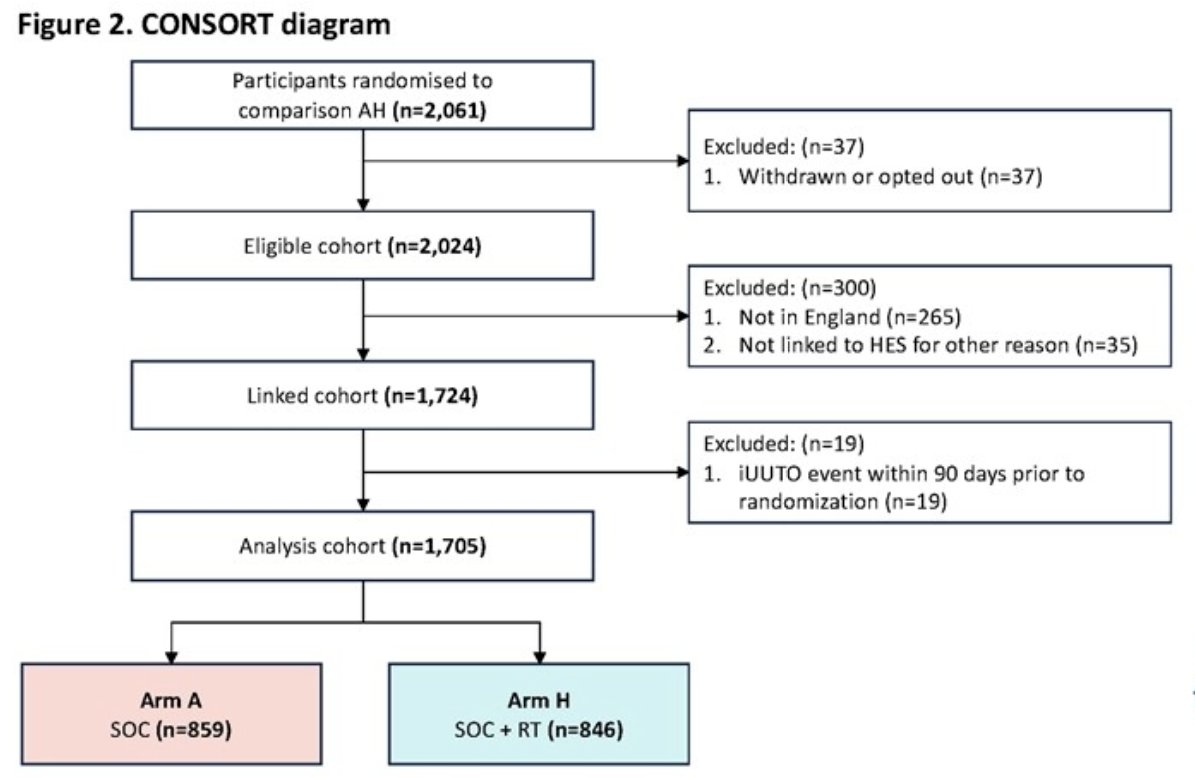
The model-based 5-year incidence of upper urinary tract obstruction requiring intervention was 5% (95% CI: 4- 7%) among patients randomized to the SOC arm and 3% (95% CI: 2- 4%) for patients in the SOC + radiotherapy arm (sHR= 0.568, 95% CI: 0.353 – 0.912, p=0.017). 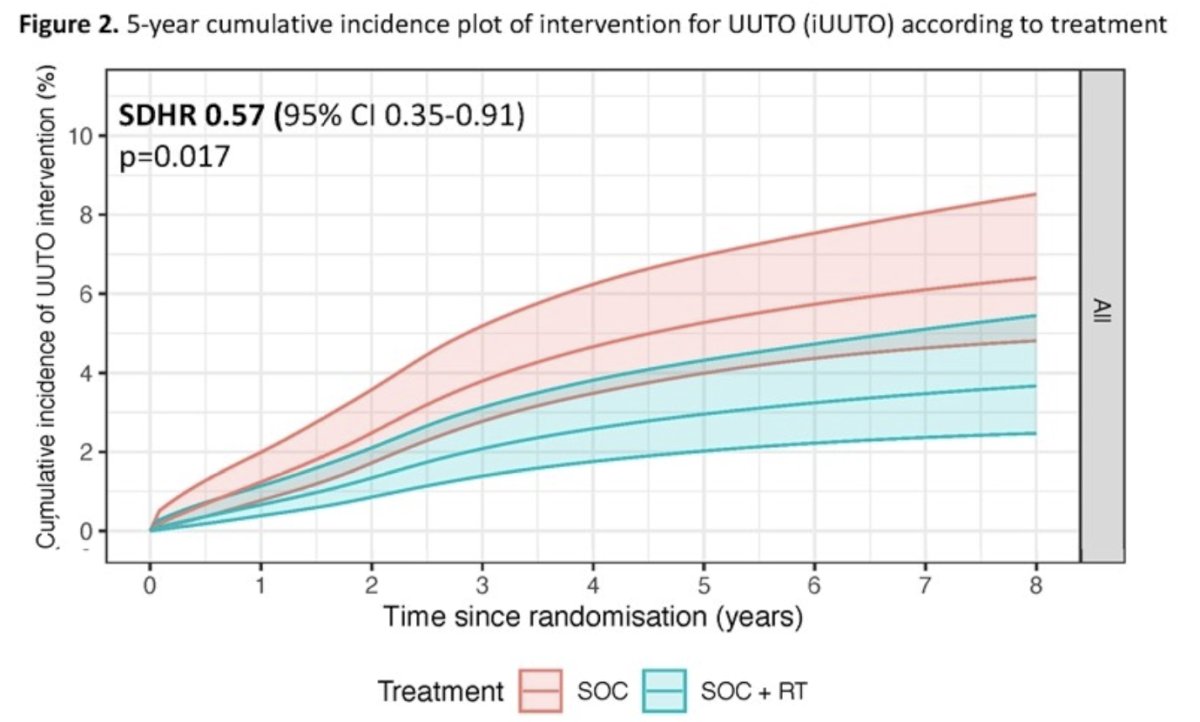
Significantly, treatment effects were comparable in both the high- and low-volume metastasis subgroups.
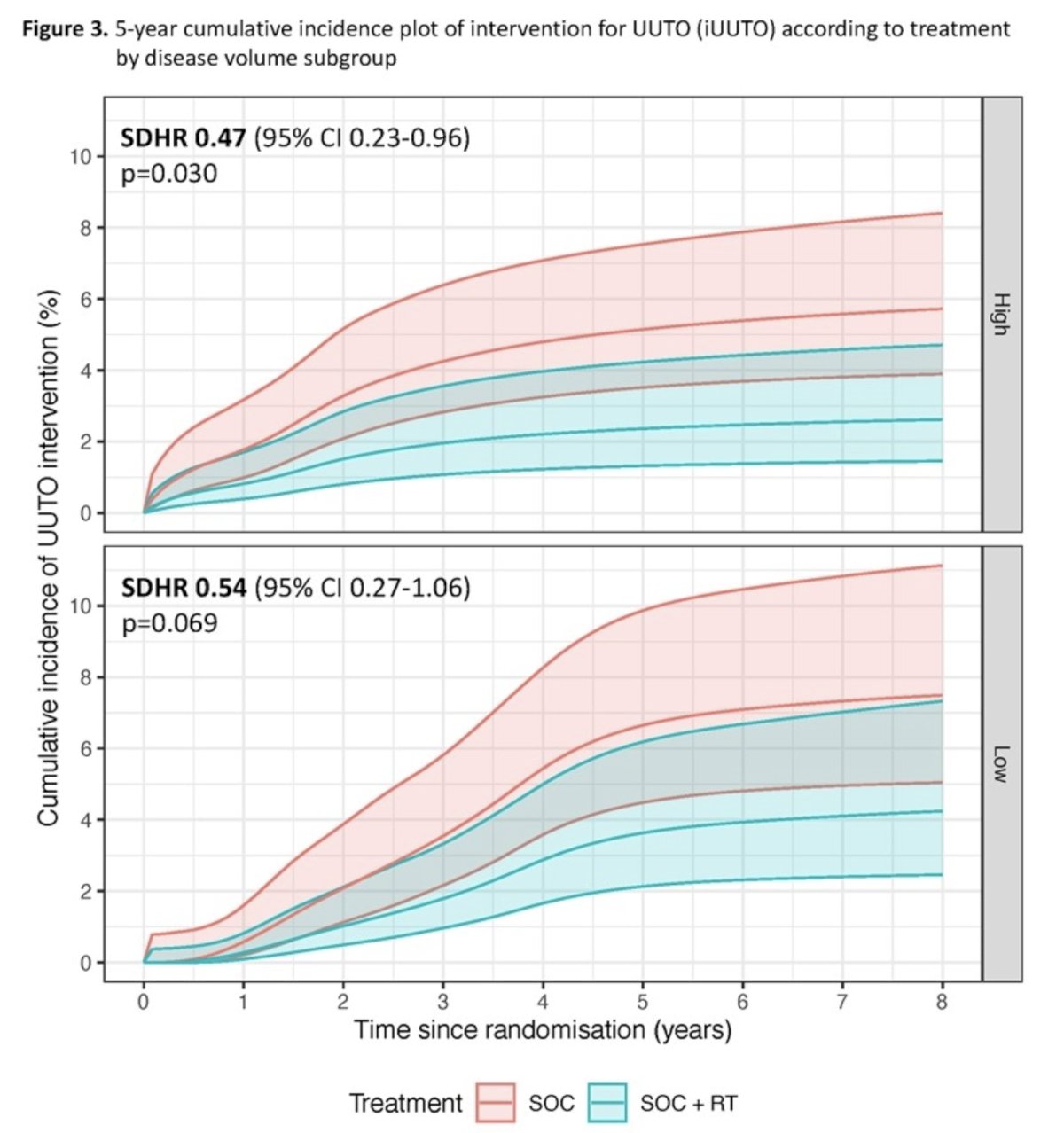
Dr. Jones and colleagues concluded that upper urinary tract obstruction-related interventions are performed in a modest proportion of mHSPC patients. Prostate radiotherapy significantly reduced the use of upper urinary tract obstruction interventions. These data support the use of prostate radiotherapy in men with mHSPC at risk of upper urinary tract obstruction.
Presented by: Craig Jones, MBChB, FRCS (Urol), MRCS, Urology SPR at Christie and Salford Royal NHS Foundation Trust, Manchester, UK
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 European Society of Medical Oncology (ESMO) Annual Congress held in Madrid, Spain between October 20th and 24th, 2023
References:
- Parker CC, James ND, Brawley CD, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. Lancet. 2018;392(10162):2353-2366.
- Parker CC, James ND, Brawley CD, et al. Radiotherapy to the prostate for men with metastatic prostate cancer in the UK and Switzerland: Long-term results from the STAMPEDE randomised controlled trial. PLoS Medicine. 2022;19(6):e1003998.


