Digestive Cancers Europe represents the patient population of Europe with digestive cancer (survivors and active cancer patients) and their families. It started with EuropaColon 14 years ago, and they have grown exponentially since then. Here is a summary of their long history and achievements, amongst others:

She focused the rest of her talk on the burden of colorectal cancer, the importance of screening and the difficulty with screening implantation.
Colon cancer burden remains quite high – it is the 3rdmost common cancer in men and 2ndin women worldwide. There are wide geographical variations in incidence – with the highest incidence in Europe and Australia/New Zealand. However, this may be due to better diagnosis and more non-cancer related competing morbidity in other countries.
Survival is also poorer in less developed regions of the world – and in poorer areas of Europe, such as central and eastern Europe.
Unlike with other cancers, there is a strong case for cancer screening in colon cancer. 1 in 4 individuals >50 years old have polyps which are pre-malignant. If caught and treated, their cancer risk of death is almost 0%. However, once they get to stage 1 cancer, their 10-year survival goes to 93%, which still isn’t bad. If they have stage 4 cancer, however, 10-year survival is between 8-10%. Therefore, early diagnosis can change the natural history of the disease.
Screening colonoscopy is the screening test of choice – it is a 30-45 minute procedure under sedation. It is a procedure and has risks, but is generally well tolerated.
The European Union has established screening guidelines for colorectal cancer. Initial guidelines were published in 2010, with an update in 2017.
However, when they looked at countries in the EU who met screening guidelines, the results were abysmal:
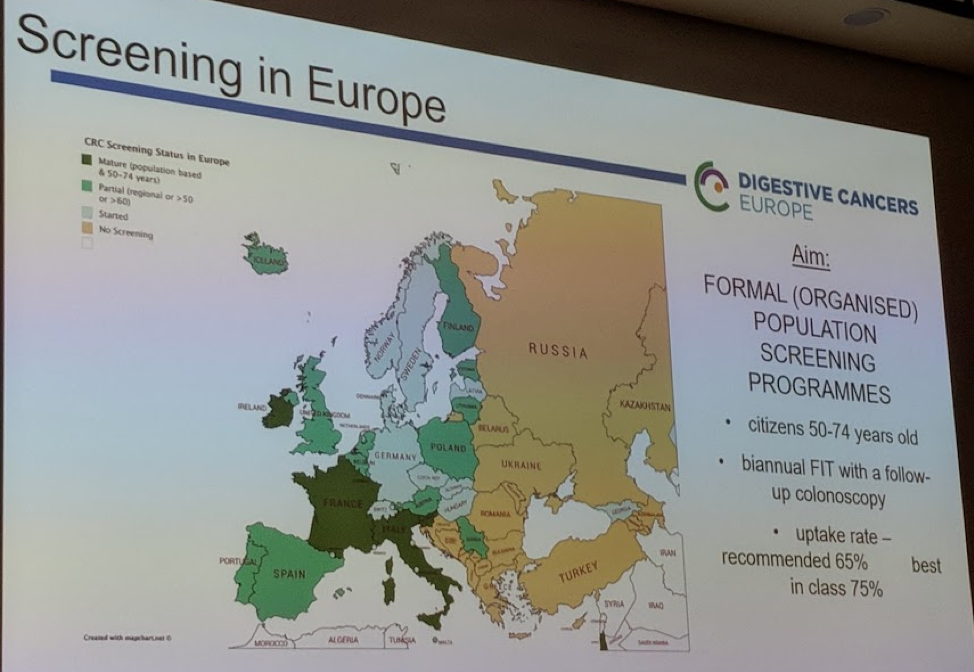
Even “mature” screening countries were only expected to have an update rate of 65% - despite that, only Ireland, France and Italy met that goal. Many countries have no screening in place at all.
Some argue against screening due to cost. While there are costs with screening each healthy patient, there are much higher costs of treating advanced colorectal cancer per patient. It is estimated that if screening is implemented, and 100% of CRC patients were diagnosed in Stage 1 or earlier, the potential savings could be $8 billion euros in medical costs annually while also saving 380,000 lives.
She ended the session by going through different screening campaigns in different countries in the EU, including France, UK, Latvia, Serbia, Portugal, Israel, and Serbia
What are the barriers to screening?
- Lack of understanding of the value of screening
- Fear of cancer (in general)
- Fear of colonoscopy
- Dislike of stool testing
- A general attitude of “I don’t have symptoms” and “I don’t have time”
- Low health literacy – especially in Eastern Europe
- An embarrassment to discuss colorectal cancer (unlike other cancers)
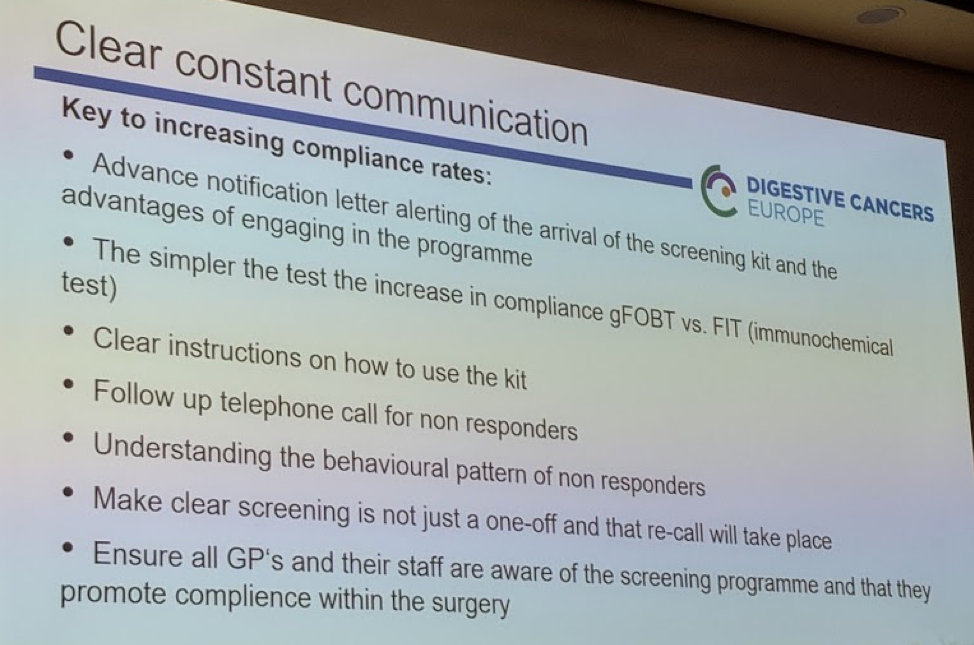
Some of her take-home points on increasing compliance rates:
Presented by: Zorana Maravic, MBA, MSc, EuropaColon
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @TjuUrology)


