The case was a 30-year-old female with a urologic history consisting of recurrent cystitis and a large retroperitoneal mass found on ultrasound during subsequent workup. Her estimated glomerular filtration rate (eGFR) was 116 ml/min/1.73m2 and her general history included an adenoidectomy and no chronic medications. The retroperitoneal mass was subsequently confirmed on CT and MRI, measuring a maximal diameter of 23 cm (cT2b). Dr. Larcher notes that there are several important issues and questions that arise in these cases:
- Do you request a preoperative renal biopsy?
- Is there any role for pre-surgical therapy?
- Do you require preoperative embolization of the tumor?
- Do you place a double J stent?
- Do you plan nephron-sparing surgery?
- Do you plan adrenal sparing surgery?
- Does minimally invasive surgery make sense?
This patient subsequently underwent selective angioembolization of the mass followed by an open laparotomy and retroperitoneal exploration. Intraoperatively, the tumor/kidney interface was small (~2cm) with no invasion of the calyceal system and thus nephron and adrenal sparing were performed, (EBL 750 cc, operative time 3 hours and 30 min). The final pathology was chromophobe renal cell carcinoma (RCC), pT2bNx, grade 2.
Dr. Ljungberg then discussed the position of performing partial nephrectomies for T2 tumors. Since there are no randomized clinical studies available, selected patients are those with a risk of impaired renal function. According to Dr. Ljungberg, mandatory reasons for performing a partial nephrectomy for a T2 kidney tumor include (i) solitary kidney, (ii) solitary functioning kidney, (iii) bilateral tumors, and (iv) multiple tumors. Several studies in this setting have demonstrated that partial nephrectomy is effective for cancer control with the advantage of preserving the kidney function but at the higher risk of complications. Furthermore, organ-sparing surgery (OSS) and cancer-specific survival (
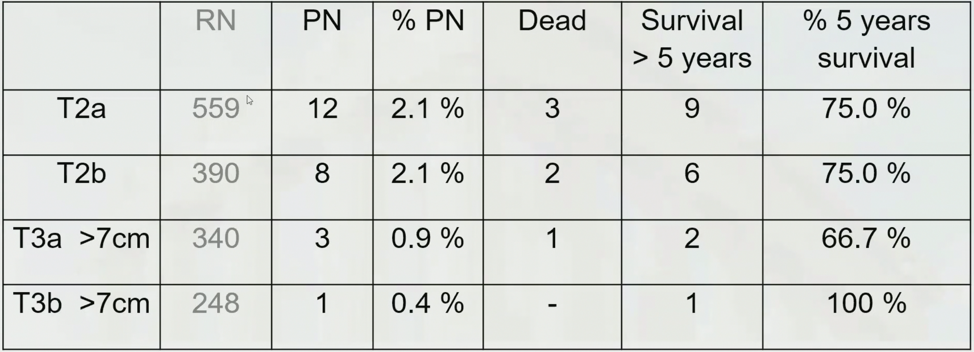
Dr. Ljungberg concluded by stating that partial nephrectomy, for patients with pT2 RCC, is an option avoiding further impairment of kidney function.
Dr. van Poppel then discussed the position of not performing partial nephrectomies for T2 tumors. According to the European Association of Urology (EAU) guidelines, Dr. van Poppel notes that patients with low-stage RCC (T1) should undergo nephron-sparing surgery rather than radical nephrectomy whenever possible. Furthermore, the guidelines suggest that for solitary renal tumors up to a diameter of 7 cm, NSS is the standard of care, whenever technically feasible. When assessing these cases it is important to consider the impact on kidney function, impact on cardiovascular events, and complication risks. Several systematic reviews suggest that partial nephrectomy confers a survival benefit and a lower risk of chronic kidney disease, but that there is “low quality of the existing evidence”, which according to Dr. van Poppel leads to a large selection bias.
In long term follow-up (median 9.3 years) of the European Organization for Research and Treatment of Cancer (EORTC) 30904 noninferiority phase 3 trial randomizing patients to NSS (n=268) or radical nephrectomy (n=273), the intention-to-treat analysis showed 10-year OS rates of 81.1% for radical nephrectomy and 75.7% for NSS. With a hazard ratio of 1.50 (95% CI 1.03-2.16), the test for noninferiority was not significant (p=0.77), and test for superiority was significant (p=0.03). However, in RCC patients and clinically and pathologically eligible patients, the difference was less pronounced (HR 1.43 and HR 1.34, respectively), and the superiority test was no longer significant (p=0.07 and p=0.17, respectively). As such, the beneficial effect of NSS on eGFR did not result in improved survival over a long median follow-up for all-cause mortality. Dr. van Poppel notes that moderate renal dysfunction arising from surgery may not have the same negative implications for overall health as when arising from medical causes such as diabetes and hypertension.
In a large meta-analysis assessing the controversial benefits of partial nephrectomy on renal function and cardiovascular outcomes, Wang et al.2 pooled 26 studies for new-onset chronic kidney disease, and 6 studies were pooled for cardiovascular outcomes. According to the pooled estimates, partial nephrectomy correlated with a 73% risk reduction of new-onset chronic kidney disease in all included patients (HR 0.27, p<0.0001) and a 65% risk reduction in patients with tumors > 4cm (HR 0.35, p<0.0001) compared with radical nephrectomy. However, there were no significant differences between groups regarding postsurgery cardiovascular events (HR 0.86, p = 0.238) and cardiovascular death (HR 0.79, p = 0.196).
With regard to complications, Dr. van Poppel notes that work from the Fox Chase Cancer Center showed that renal mass complexity predicts rates of major complications following partial nephrectomy.3 Among 390 patients undergoing partial nephrectomy for low- (28%), moderate- (55.6%), and high-complexity (16.4%) tumors, minor complication rates were comparable (26.6 vs. 24.9 vs 32.8%; p=0.45), whereas major complication rates differed (6.4 vs. 11.1 vs. 21.9%; p=0.009) among tumor complexity groups. Thus, recommending partial nephrectomy to all patients for whom the operation is technically feasible exposes a subgroup of patients to increased perioperative risks.
Presented by: Alessandro Larcher, MD, Universite Vita-Salute San Raffaele, Milan, Italy; Borje Ljungberg, MD, PhD, Umea University, Umea, Sweden; and Hein van Poppel, MD, PhD, University Hospital K.U. Leuven, Leuven, Belgium
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md at the 12th European Multidisciplinary Congress on Urological Cancers (EMUC) (#EMUC20 ), November 13th - 14th, 2020
References:
- Van Poppel H, da Pozzo L, Albrecht W, et al. A prospective, randomized EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol 2011 Apr;59(4):543-552.
- Wang Z, Wang G, Xia Q, et al. Partial nephrectomy vs. radical nephrectomy for renal tumors: A meta-analysis of renal function and cardiovascular outcomes. Urol Oncol 2016 De;34(12):533.
- Simhan J, Smaldone MC, Tsai KJ, et al. Objective measures of renal mass anatomic complexity predict rates of major complications following partial nephrectomy. Eur Urol 2011 Oct;60(4):724-730.


