(UroToday.com) In the eleventh session of the 2022 International Kidney Cancer Symposium (IKCS): Europe meeting focusing on the role of radiotherapy for kidney cancer, Dr. Flippot highlighted treatment approaches for patients with brain metastases from renal cell carcinoma (RCC).
To begin, he emphasized that brain metastasis may be found in up to one in ten patients with metastatic RCC and, of these, one-third may be diagnosed prior to first-line therapy. In general, brain metastases are found in the context of aggressive disease features such as sarcomatoid histology, a large primary tumor, and evidence of extra-abdominal disease dissemination. In the era of tyrosine kinase inhibitors, to date, patients diagnosed with brain metastases have a dismal prognosis with most having overall survival of less than 12 months. Therefore, identifying efficacious treatment approaches is a priority. To this end, Dr. Flippot described the available evidence for treatment approach which do and do not appear to be effective.
He first discussed stereotactic radiotherapy which provides good local control, with one year rates of local control exceeding 90% for patients with smaller isolated brain metastasis (<30 mm). However, distant failure is relatively common and is seen more frequently in patients with multifocal disease. Thus, systemic therapy approaches, in combination with stereotactic radiotherapy, are warranted. Unfortunately, as he highlighted sunitinib (which until recently was the standard of care) does not appear to be effective based on limited available data. In a single phase 2 trial of 16 patients, none had evidence of intracranial response and the time to progression was only 2 months.
In the context of the NIVOREN trial, Dr. Flippot and colleagues examined the efficacy of nivolumab monotherapy in patients with brain metastases who had not previously received brain radiotherapy. While the intracranial response rate was 12%, all responders had a single lesion measuring less than 1 cm. Further, time to intracranial progression was only 2.7 months suggesting that this systemic therapy approach alone is unlikely to control intracranial disease.
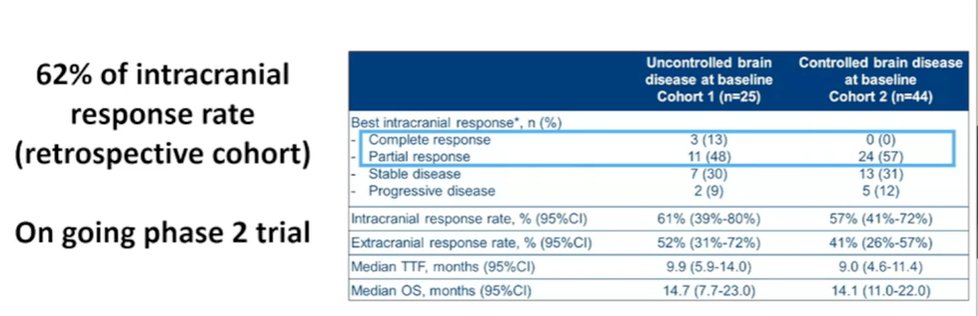
However, somewhat promisingly, a multi-center retrospective cohort study of cabozantinib has demonstrated an intracranial response rate of 62%. These results have prompted a currently ongoing phase II trial in France to assess role of cabozantinib in patients with brain metastasis from RCC.
While monotherapy was standard of care for many years, combination treatment approaches are now the accepted first-line treatment for most patients. Unfortunately, subgroup and post hoc analyses of JAVELIN Renal 101 and CheckMate 920 have demonstrated relatively sobering results. In JAVELIN Renal 101, the median progression free survival for patients with brain metastasis receiving avelumab and axitinib was 4.9 months, compared with 13.8 in the overall cohort, though this was somewhat better than among those who received sunitinib (2.8 months). In CheckMate 920, median progression-free survival was promisingly 9 months among 28 included patients though 25% had early intracranial progression.
Given that we likely want to administer both stereotactic radiotherapy and systemic therapy, the next question is how we sequence treatment approaches. Again utilizing data from the NIVOREN real world registry with a subgroup of patients with brain metastasis, Dr. Flippot highlighted that there was a better intracranial progression free survival at the time of nivolumab initiation for those patients who had previously received brain radiotherapy (hazard ratio 0.49). Further, these patients were less likely to have symptoms associated with their brain metastases and were less likely to require subsequent focal brain therapy.

Thus, he advocated that radiotherapy should be administered prior to initiating systemic therapy. Further, he suggested that routine use of brain MRI should be considered. When considering systemic therapy choices, he noted that cabozanitinib should potentially be given preference either as monotherapy or in combination, particularly in situations where local therapy is challenging.
However, moving forward to be able to better treat these patients, he highlighted the importance of prospective data (including the CABRAMET trial of single agent cabozantinib), utilizing multi-center data to understand this condition, work to better understand the biologic determinants of brain metastasis, and finally, assessment of non-clear cell histologies.
Presented by: Ronan Flippot, MD, MSc, Institut de Cancérologie Gustave Roussy


