Dr. Walz concluded this session and began his talk stating the goals of RP. These include:
1. Cancer control
2. Urinary continence
3. Preservation of erectile function
It is important to remember that the nerves pass laterally to the prostate, but also laterally to the seminal vesicles (SVs). Therefore, when dissecting the SVs, care must be taken not to damage the adjacent nerves. The nerves pass near the prostate apex, and near the urethra, so care must be taken in this vicinity as well.
The relevant cavernous nerves pass all around the prostate, with 46-66% of them being at the 4-6 o’clock sector, and 21-29% passing along the 1-3 o’clock sector (Figure 1).

Figure 1 – Anatomy of the nerves at the prostate:
Furthermore, there is great variability of the periprostatic fascia location and the nerves within it (Figure 2).

Figure 2 – Variability of the periprostatic fascia:
Dr. Walz moved on to discuss the dissection planes for NS, mentioning the intrafascial plane for complete NS, the interfascial plane for partial NS, and the extrafascial plan for no NS (Figure 3).
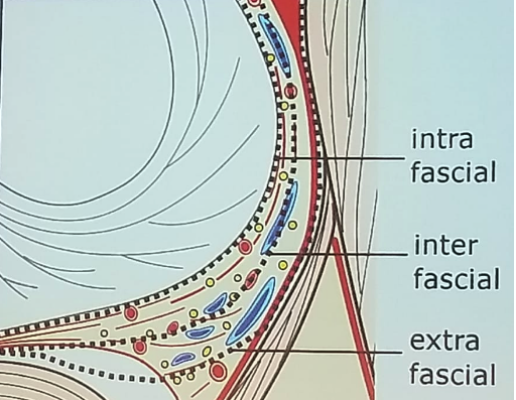
Figure 3 – Dissection planes for nerve-sparing:
There has been a substantial evolution in the standardization of NS over the years, as can be seen in figure 4.

Figure 4 – Dissection planes and nerve-sparing grading:
The anatomy of the pelvic floor is also extremely important. It is relevant for continence, especially the anterior parts of levator ani (M. puboperinealis), originating from the pubic bone and inserting into the central tendon. The continence system consists of two parts: the bladder and the urethral sphincter. The urethral sphincter is composed of a striated muscle which is horseshoe or omega-shaped, adjacent to the m. puboperinealis, and the smooth muscle sphincter, which has two parts. These include the outer circular element and the inner longitudinal element. The location and shape of the smooth muscle part of the sphincter strongly depend on the apical shape. The sphincter is innervated by nerves located at the 3-5 o’clock and 7-9 o’clock position, 3-13 mm caudal to the prostate apex. Its preservation is critical for maintaining continence.
Presented by: Jochen Walz, Marseille, France
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the EAU Robotic Urology Section (ERUS) Meeting - September 5 - 7, 2018 - Marseille, France


