(UroToday.com) The 2023 EAU annual meeting included a joint session of the EAU and the Advanced Prostate Cancer Consensus, featuring a presentation by Dr. Bertrand Tombal (after Dr. Van Oort was unable to present at the last minute) discussing how among patients with high-risk localized disease, M0 on conventional imaging but one bone lesion on PSMA PET/CT, we should be treating these patients with surgery +/- radiotherapy +/- systemic treatment.
Dr. Tombal started by highlighting two 18F-DCFPyL PSMA PET/CT staging trials. The first was the SALT trial, a prospective multi-center study assessing detection of pelvic lymph nodes.1 Among 117 men undergoing PSMA PET/CT prior to extended pelvic lymph node dissection, detection of lymph node metastases had a high specificity (94.0%), but limited sensitivity. Similar results were seen in the United States’ OSPREY2 trial (n = 252), with a median specificity of 97.9% and median sensitivity of 40.3%. With regards to staging with 68Ga-PSMA PET/CT, van Kalmthought et al.3 prospectively assessed 103 men (97 underwent extended pelvic lymph node dissection) of which 42.3% had lymph node metastases. The per-patient sensitivity was 41.5% and per patient specificity was 90.9%, with a 12.6% treatment change rate. In 2018, Corfield et al.4 performed a systematic review of 12 studies (n = 322) that used 68Ga-PSMA PET/CT for staging. There was good per lesion specificity of 82-100% and per patient 67-99%. However, there was high variability in sensitivity for initial staging (33-99%), per lesion analysis (33-92%), and per patient analysis (66-91%). In most studies, there was increased detection rates to conventional imaging modalities (ie. bone and CT scan).
The proPSMA study was an Australian multi-center, two-arm randomized controlled staging trial of men with histologically confirmed prostate cancer who were being considered for curative intent radical prostatectomy or radiotherapy.2 There were 302 patients randomized to either conventional imaging (n = 152) or 68Ga-PSMA-11 PET/CT (n = 150). PSMA PET/CT had a 27% absolute greater AUC for accuracy compared to conventional imaging (95% CI for difference: 23 – 31%): 92% (95% CI: 88 – 95%) vs. 65% (95% CI: 60 – 69%). Conventional imaging had both a lower sensitivity (38% vs. 85%) and specificity (91% vs. 98%). Subgroup analyses by site of metastasis demonstrated the superiority of PSMA PET/CT for pelvic nodal (AUC: 91% versus 59%) and distant metastases (AUC: 95% versus 74%):
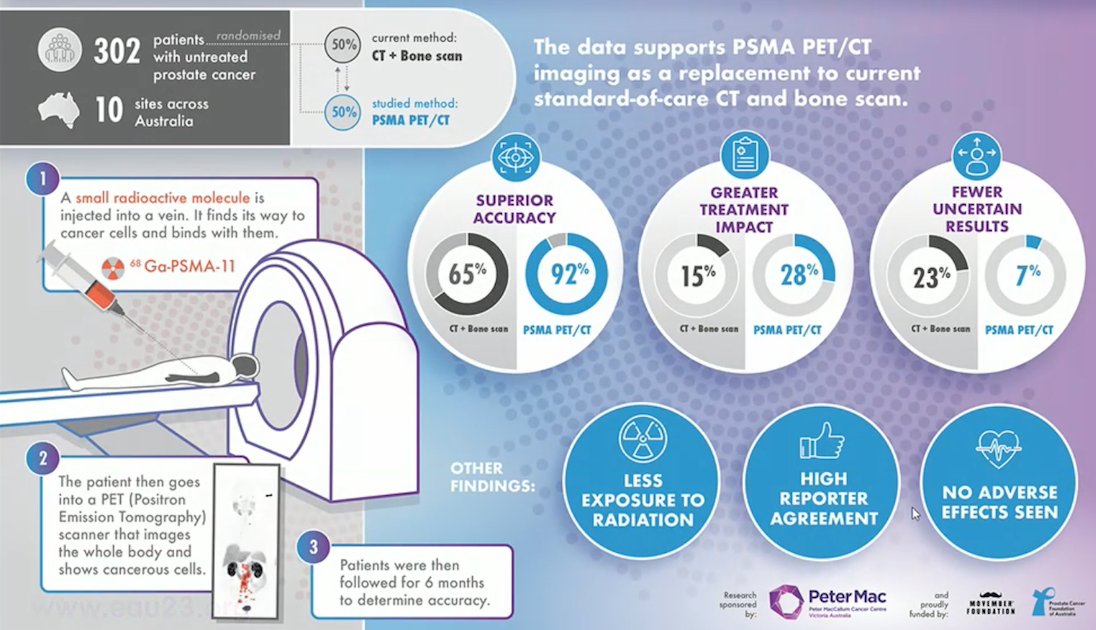
With regards to treatment change in proPSMA, 14% went from a curative treatment to palliative approach, and 14% changed from a surgical approach to a radiotherapy technique.
Dr. Tombal then discussed several key questions asked to the APCCC 2022 experts: For patients with high-risk localized prostate cancer for whom radical local treatment (prostatectomy or radiotherapy) of the primary tumor is planned, if patients are staged as N0M0 on conventional imaging but are found to have 1-3 PSMA PET-positive lesions in the bone (M1) what are you most likely to do? The most common answer was metastasis-directed therapy and systemic therapy at 51%:

As noted above, there was no consensus for any answer option, but a combined total of 96% of panelists voted for a treatment change. The next question was: For patients with high risk localized prostate cancer for whom radical local treatment (prostatectomy or radiotherapy) of the primary tumor is planned, if they are staged as N0M0 on conventional imaging but are found to have >=4 PSMA PET positive lesions in the bone (M1) what are you most likely to do? The most common answer was to intensify treatment by adding systemic therapy:

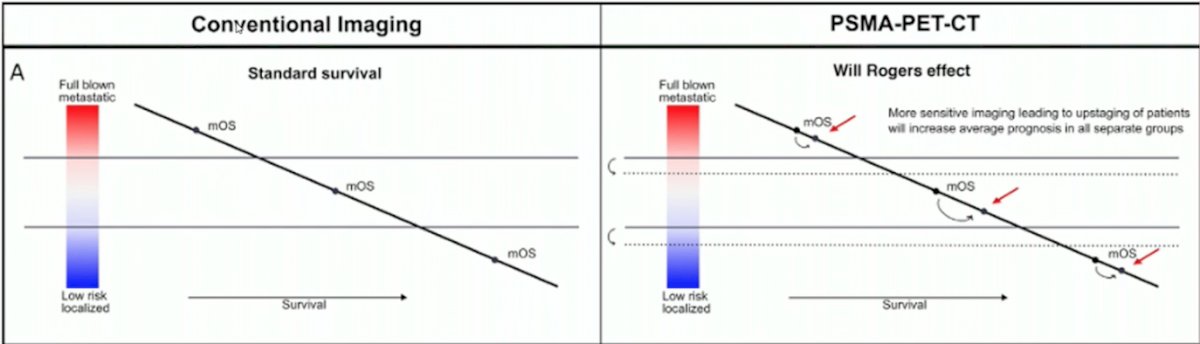
Dr. Tombal notes that the biological and clinical importance remains unknown for patients planned for radical treatment who subsequently have a PSMA PET/CT and whose treatment is changed to palliative intent or they receive less radical treatment due to small distant metastases. Denying and switching to palliative therapy is denying a potential chance to cure. Conventional imaging and PSMA PET/CT can be summarized in the following figure, highlighting the Will Rogers effect of stage migration for PSMA PET/CT:
Dr. Tombal concluded his presentation with the following take-home messages, summarizing several key points in the EAU guidelines:
- PSMA PET/CT is more accurate for staging than CT and bone scan for high-risk disease, but to date no outcome data exist to inform subsequent patient management (Level of evidence: 1b)
- For high-risk localized disease/locally advanced disease:
- Perform metastatic screening including at least cross-sectional abdominopelvic imaging and a bone scan (Strength rating: Strong)
- When using PSMA PET or whole body MRI to increase sensitivity, be aware of the lack of outcome data of subsequent treatment changes (Strength rating: Strong)
Presented by: Bertrand Tombal, MD, PhD, Cliniques Universitaires Saint Luc, UCLouvain, Brussels, Belgium
Slide preparation: Inge M. Van Oort, MD, PhD Nijmegen, The Netherlands
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 European Association of Urology (EAU) Annual Meeting, Milan, IT, Fri, Mar 10 – Mon, Mar 13, 2023.
References
- Jansen BHE, Bodar YJL, Zwezerijnen GJC, et al. Pelvic lymph-node staging with 18F-DCFPyL PET/CT prior to extended pelvic lymph node dissection in primary prostate cancer – the SALT trial. Eur J Nucl Med Mol Imaging. 2021 Feb;48(2):509-520.
- Pienta KJ, Gorin MA, Rowe SP, et al. A Phase 2/3 Prospective Multicenter Study of the Diagnostic Accuracy of Prostate Specific Membrane Antigen PET/CT with 18F-DCFPyL in Prostate Cancer Patients (OSPREY). J Urol. 2021 Jul;206(1):52-61.
- van Kalmthought LWM, van Melick HHE, Lavalaye J, et al. Prospective validation of Gallium-68 Prostate Specific Membrane Antigen Positron Emission Tomography/Computerized Tomography for primary staging of prostate cancer. J Urol. 2020 Mar;203(3):537-545.
- Corfield J, Perera M, Bolton D, et al. 68Ga-prostate specific membrane antigen (PSMA) positron emission tomography (PET) for primary staging of high-risk prostate cancer: A systematic review. World J Urol. 2018 Apr;36(4):519-527.
- Hofman MS, Lawrentschuk N, Francis, RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): A prospective, randomized, multicentre study. Lancet 2020 Apr 11;395(10231):1208-1216.
Related Content:
Eva Comperat EAU 2023: Patient with High-Risk Localized Disease, M0 on Conventional Imaging but One Bone Lesion on PSMA PET/CT: Subtypes of Prostate Cancer and How They Change our Management
Thomas Zilli EAU 2023: Patient with High-Risk Localized Disease, M0 on Conventional Imaging but One Bone Lesion on PSMA PET/CT: Arguments for a Radiotherapeutic Approach +/- Systemic Treatment
Maria De Santis EAU 2023: Patient with High-Risk Localized Disease, M0 on Conventional Imaging but One Bone Lesion on PSMA PET/CT: Systemic Therapy: What and for how long?
Alicia Morgans EAU 2023: Patient with High-Risk Localized Disease, M0 on Conventional Imaging but One Bone Lesion on PSMA PET/CT: How to Treat a Frail and Elderly Patient in this Situation


