(UroToday.com) The 2023 EAU annual meeting included a session on clinically meaningful questions in the management of advanced, hormone-sensitive prostate cancer, featuring a state-of-the-art presentation by Dr. Henk G. van der Poel discussing how PSMA-PET has revolutionized the management of hormone-sensitive prostate cancer.
Dr. van der Poel started by highlighting that 2023 is the 40th birthday of PSMA, initially discovered by Horoszewicz in 1983 and further characterized by Fair in 1993. As we know, PSMA is expressed in the primary tumor and in sites of metastases, as well as overexpressed in high grade prostate cancer. So, is PSMA PET/CT the Holy Grail? More specifically, what are the implications of better staging versus over/under treatment. Dr. van der Poel notes that imaging is the basis of all oncological management:
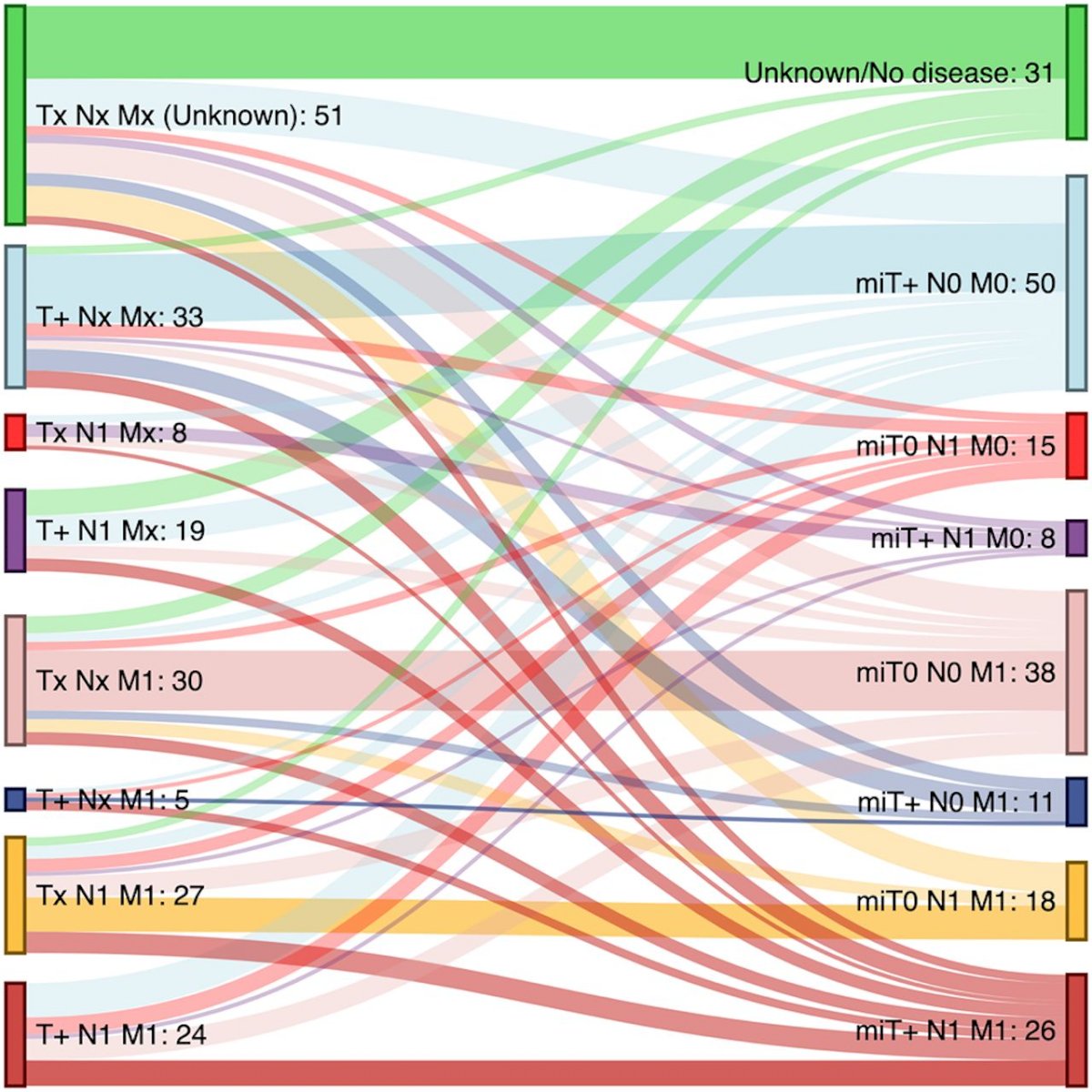
Dr. Van der Poel started by discussing some of the literature surrounding PSMA PET/CT and staging in high risk patients. Data from Sonni et al.] looking at 68Ga-PSMA-11 for restaging found that among 197 patients, 69% of men had a change in staging, including 38% that were upstaged and 30% that were downstaged:1
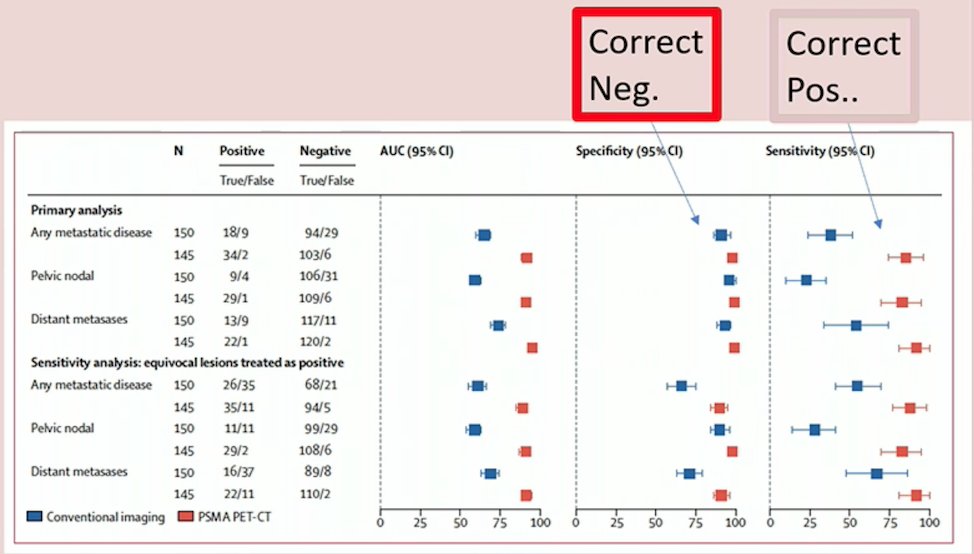
The proPSMA study was an Australian multi-center, two-arm randomized controlled staging trial of men with histologically confirmed prostate cancer who were being considered for curative intent radical prostatectomy or radiotherapy.2 There were 302 patients randomized to either conventional imaging (n = 152) or 68Ga-PSMA-11 PET/CT (n = 150). PSMA PET/CT had a 27% absolute greater AUC for accuracy compared to conventional imaging (95% CI for difference: 23 – 31%): 92% (95% CI: 88 – 95%) vs. 65% (95% CI: 60 – 69%). Conventional imaging had both a lower sensitivity (38% vs. 85%) and specificity (91% vs. 98%). Subgroup analyses by site of metastasis demonstrated the superiority of PSMA PET/CT for pelvic nodal (AUC: 91% versus 59%) and distant metastases (AUC: 95% versus 74%):
A Danish staging study assessed 68Ga-PSMA in 691 men, with a specificity of 97% and 1 in 6 men having M1b disease [3]. However, sensitivity for nodal metastases per patient was only 31% (median 7 mm detected, 3 mm (IQR 2-11) non-detected):
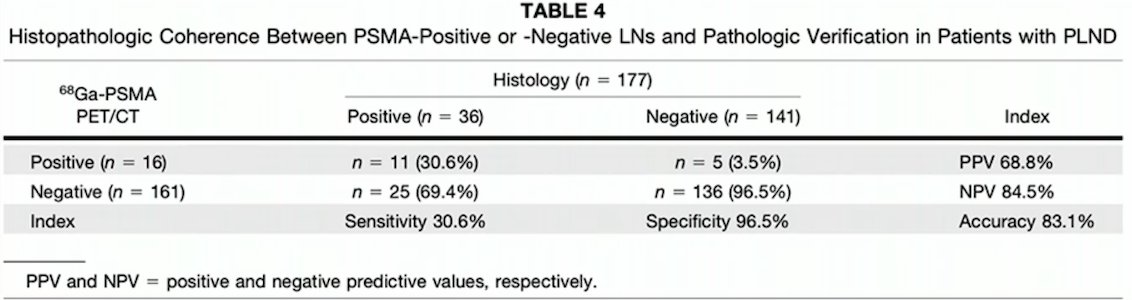
The two US-based studies in this disease space were the UCSF/UCLA study of 68Ga-PSMA-11 (n = 277) [4] and the OSPREY study of 18F-DCFPyL (n = 385) [5]. Both of these studies confirmed an overall high specificity (98%), but also a low sensitivity for pN+ disease (40% in both studies). With regards to negative predictive value for PSMA PET/CT, this is ~88%, more specifically 92% for intermediate risk disease and 83% for high risk disease. Of note, PSMA PET may improve prediction of nodal metastases when added to nomograms.
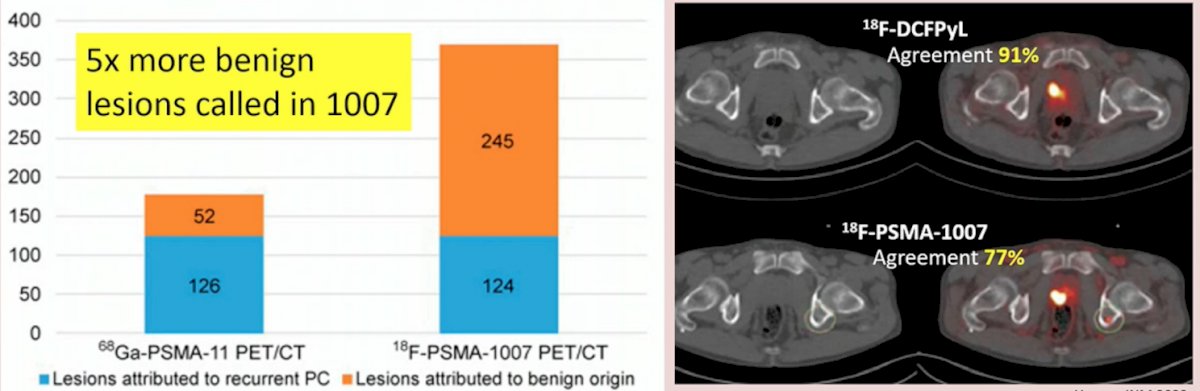
Currently, there are two approved tracers, 68Ga-PSMA-11 and 18F-DCFPyL, both of which have kidney dominated excretion. Importantly, the not yet approved 18F-PSMA-1007 has liver dominated excretion, thus potentially being more useful for detection of local recurrences. However, 18F-PSMA-1007 has been noted to have a considerably higher number of benign lesions detected compared to 68Ga-PSMA-11, as well as poorer inter-reader agreement:
Adequate delineation of bone metastases is important in staging, particularly for medical oncologists when determining high versus low volume disease. In this setting, the sensitivity of PSMA PET/CT is 90-95% compared to bone scan, which is 70-83%. Furthermore, PSMA PET/CT has been reported to be positive in 10% of cases when bone scan is negative, and also detects 20% more bone metastases compared to bone scans.
The crux of the matter with regards to staging is the somewhat poor performance of 68Ga-PSMA-11 and 18F-DCFPyL for lymph node detection, given that 60% of nodal metastases are missed on PSMA PET/CT. Additionally, false positives may also be an issue, particularly when it comes to rib lesions, which are often fractures, hemangiomas, and/or dysplasia. Thus, the 2023 prostate cancer guidelines for PSMA in primary staging state that “Treatment should not be changed based on PSMA PET/CT findings” (Strength rating: Strong) and we should only be obtaining these images if we think the findings may change our management.
Dr. van der Poel highlighted that PSMA is becoming more and more prominent in our discussions about prostate cancer, noting that in the most recent update from the APCCC conference, PSA was mentioned 181 times and PSMA was mentioned 182 times. Additionally, the following consensus statements were made at the APCCC 2022 conference:
- Do you recommend PSMA PET in the majority of patients with clinically localized high-risk prostate cancer? 77% responded Yes
- Are you in favor of refining the metastatic classification (N and M) in TNM staging to have a notation for PSMA PET-positive lesions? 87% responded Yes
- In the majority of patients with clinically localized prostate cancer and PSMA positivity, with metastasis-consistent findings in the bone on the CT of upfront PSMA PET, do you recommend any additional imaging (ie. MRI or bone scan)? 78% responded No
Where PSMA PET/CT has made substantial headway is in the recurrent disease space. Summarizing the available literature, Dr. van der Poel notes that PSMA PET/CT (i) is able to detect recurrence in 40% of patients at a PSA as low as 0.2 ng/mL, (ii) it improves outcomes after salvage radiotherapy, and (iii) in patients with a rising PSA after external beam radiotherapy, 75% of lesions are detected before the patient’s PSA reaches the Phoenix criteria for recurrence. However, the EAU guidelines provide a “weak recommendation for PSMA PET in recurrence”.
Dr. van der Poel notes that PSMA may be intoxicating in that it out performs CT/bone scan for staging and is helpful to guide treatment options in recurrent disease, however it can also be sobering in that it only detects lesions at the level of 4 mm (>2,000,000 prostate cancer cells). False positive results are not uncommon, thus requiring a reader with great expertise. Currently there are 182 ongoing trials, and one of the biggest questions at the moment is: Will management change and improve outcomes?
Dr. van der Poel concluded his presentation discussing PSMA-PET in the management of hormone-sensitive prostate cancer with several ‘To-Dos’ and a quote from the famous Italian physicist Enrico Fermi:
- PSMA PET/CT has high positive predictive value for cN1
- A single M1 lesion must be confirmed
- Detection/treatment of oligometastases may reduce progression
- In recurrent disease, PSMA lesion detection improves salvage radiotherapy outcomes
- “Before I came here I was confused about the subject. Having listened to your lecture I am still confused. But on a higher level.”
Presented by: Henk G. van der Poel, The Netherlands Cancer Institute-Antoni van Leeuwenhoek Hospital Amsterdam, The Netherlands
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 European Association of Urology (EAU) Annual Meeting, Milan, IT, Fri, Mar 10 – Mon, Mar 13, 2023.References:
- Sonni I, Eiber M, Fendler WP, et al. Impact of 68Ga-PSMA-11 PET/CT on Staging and Management of Prostate Cancer Patients in Various Clinical Settings: A Prospective Single-Center Study. J Nucl Med. 2020 Aug;61(8):1153-1160.
- Hofman MS, Lawrentschuk N, Francis, RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): A prospective, randomized, multicentre study. Lancet 2020 Apr 11;395(10231):1208-1216.
- Klingenberg S, Jochumsen MR, Ulhoi BP, et al. 68Ga-PSMA PET/CT for Primary Lymph Nodes and Distant Metastasis NM Staging of High-Risk Prostate Cancer. J Nucl Med. 2021 Feb;62(2):214-220.
- Hope TA, Eiber M, Armstrong WR, et al. Diagnostic Accuracy of 68Ga-PSMA-11 PET for Pelvic Nodal Metastasis Detection Prior to Radical Prostatectomy and Pelvic Lymph Node Dissection: A Multicenter Prospective Phase 3 Imaging Trial. JAMA Oncol. 2021 Nov 1;7(11):1635-1642.
- Pienta KJ, Gorin MA, Rowe SP, et al. A Phase 2/3 Prospective Multicenter Study of the Diagnostic Accuracy of Prostate Specific Membrane Antigen PET/CT with 18F-DCFPyL in Prostate Cancer Patients (OSPREY). J Urol. 2021 Jul;206(1):52-61.


