Dr. Baboudjian began by presenting the clinical case of a:
- 54-year-old male
- Caucasian
- Age-adjusted Charlson comorbidity index of 1
- Medical history
- Personal: hypertension (on amlodipine), no prior surgery
- Family: father with de novo metastatic prostate cancer at 67 years, now deceased
- Mild lower urinary tract symptoms (IPSS: 6/35) and sexually active (IIEF-5: 24/25)
 In 2023, now 54 and with a PSA of 9.21 (DRE normal throughout) and a PSA density of 0.18, the patient underwent a PSMA-PET/CT with positive findings in the left apex transition zone. The patient subsequently underwent a systematic + targeted biopsy with findings of two positive cores of ISUP grade 2, albeit with 10% pattern 4 disease.
In 2023, now 54 and with a PSA of 9.21 (DRE normal throughout) and a PSA density of 0.18, the patient underwent a PSMA-PET/CT with positive findings in the left apex transition zone. The patient subsequently underwent a systematic + targeted biopsy with findings of two positive cores of ISUP grade 2, albeit with 10% pattern 4 disease.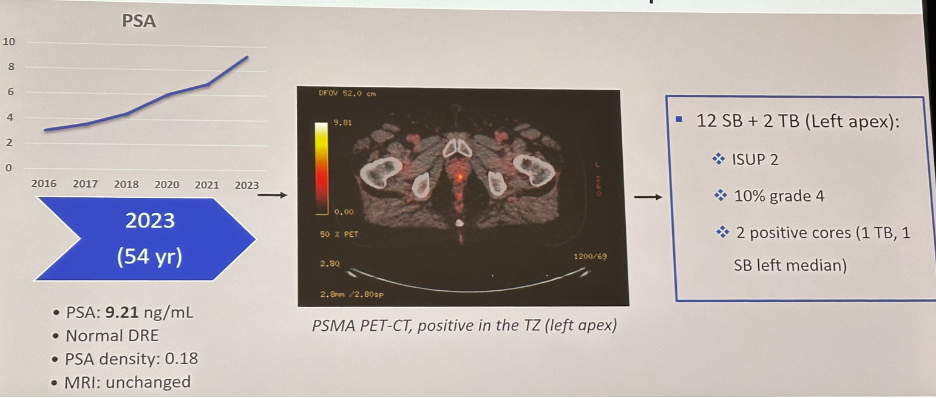
At this point, the presentation was turned over to Dr. Hofman to discuss the emerging role of PSMA-PET/CT in supplanting mpMRI for prostate cancer detection.
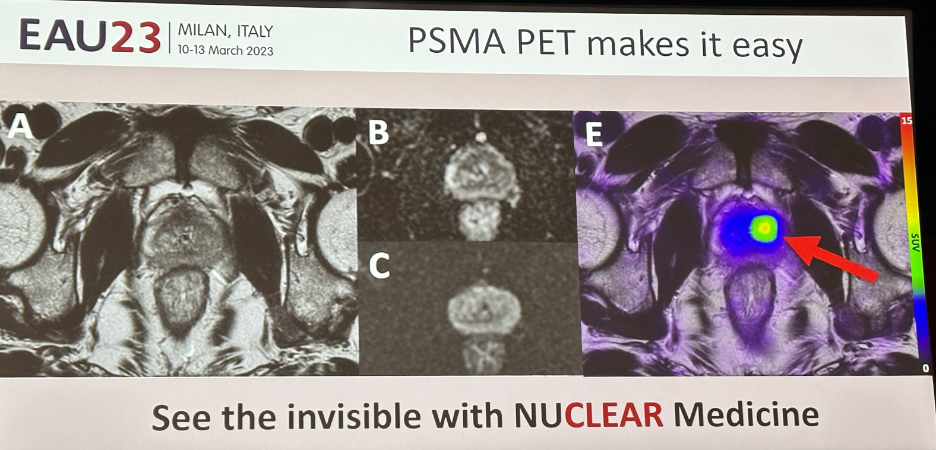
While lesion scoring systems, as demonstrated in the PRIMARY trial, continue to evolve, Dr. Hofman believes that interpretation of PSMA-PET/CT images is significantly easier compared to mpMRI, as demonstrated in the example below:
 The PRIMARY trial was a prospective multicenter phase II imaging trial that enrolled men with suspected PCa, no prior biopsy, and a recent mpMRI examination within 6 months, and for whom prostate biopsy was planned. In total, 291 men underwent an mpMRI, 68Ga-PSMA PET/CT, and systematic biopsy with or without targeted biopsy.
The PRIMARY trial was a prospective multicenter phase II imaging trial that enrolled men with suspected PCa, no prior biopsy, and a recent mpMRI examination within 6 months, and for whom prostate biopsy was planned. In total, 291 men underwent an mpMRI, 68Ga-PSMA PET/CT, and systematic biopsy with or without targeted biopsy. 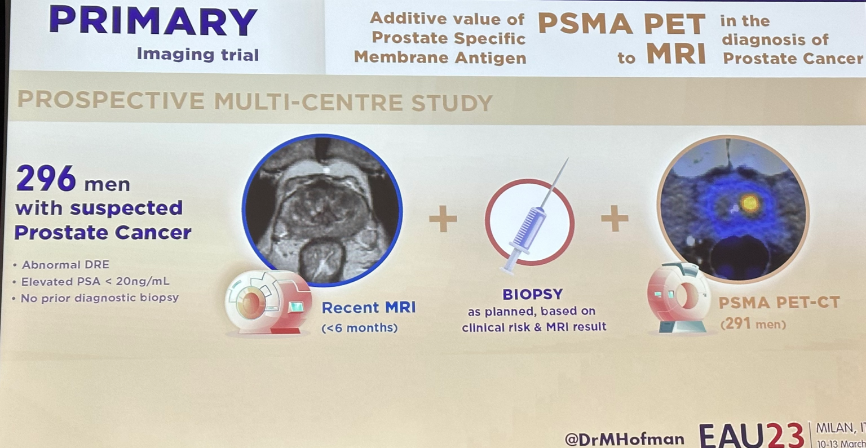
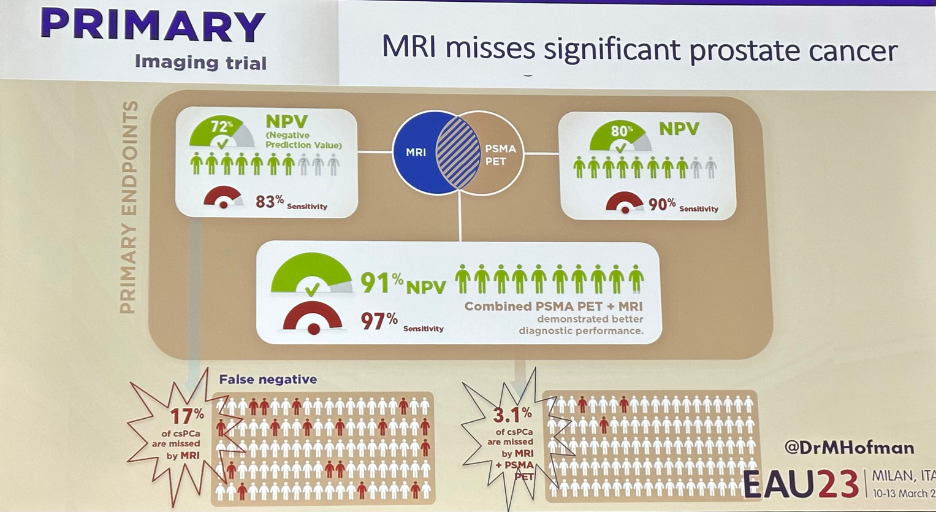
A combined mpRMI + PSMA-PET/CT approach improved the sensitivity from 83% with MRI alone to 97% when combined (NPV: 72% to 91%), at the expense of decreased specificity (53% reduced to 40%). Significantly, a combination approach reduced the false negative rate for detection of csPCa from 17% to 3.1%.1
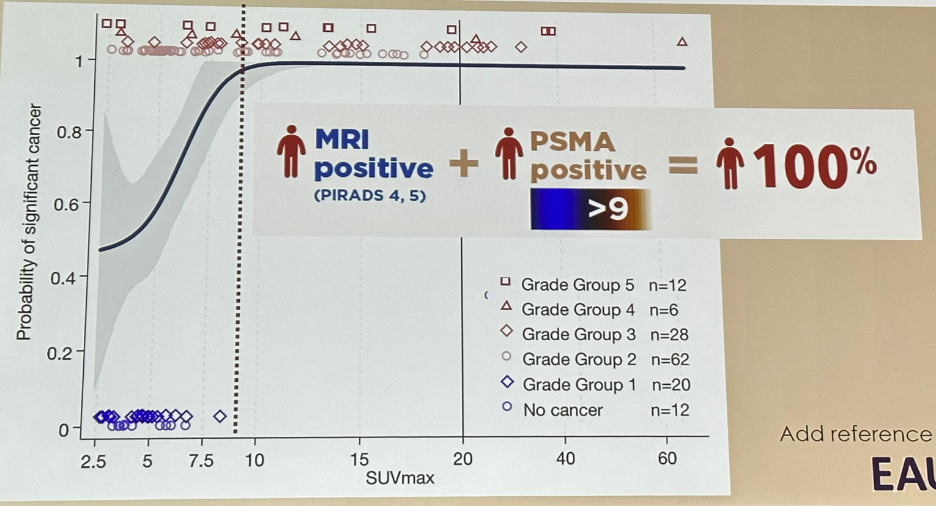
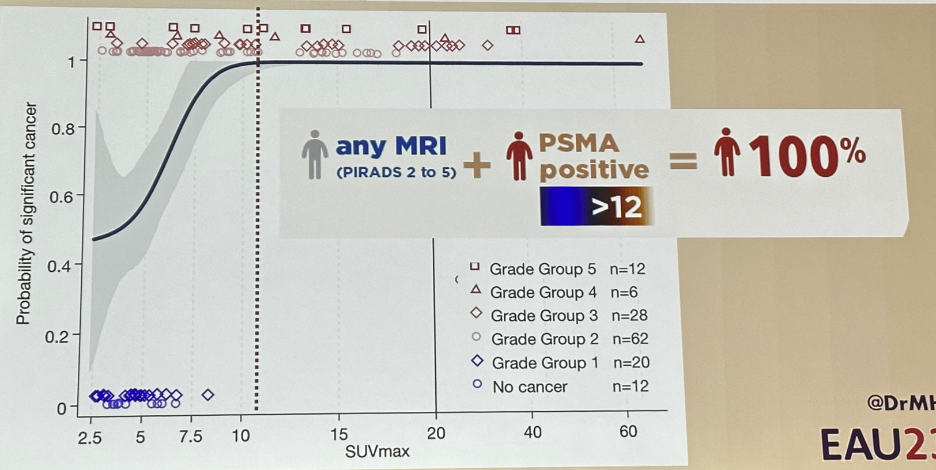
Interestingly, there was a direct correlation between the SUVmax level and increased/worsening ISUP grade group disease. The probability of csPCa increased exponentially as the SUVmax increased from 2.5 to 10, with the probability of csPCa levelling off at 1.0 for lesions/patients with SUVmax of 10 or greater.

Can PSMA-PET/CT replace biopsy? In other words, can the positive predictive value of a PSMA-PET/CT, either alone or in combination, produce a PPV for csPCa of 100%? Among patients with an MRI positive lesion (PIRADS 4/5) and a PSMA positive scan with an SUVmax of >9, the PPV for csPCa was 100%.
A similar PPV of 100% was observed when patients had any MRI (PIRADS 2/3) and a PSMA positive scan with an SUVmax of >12.
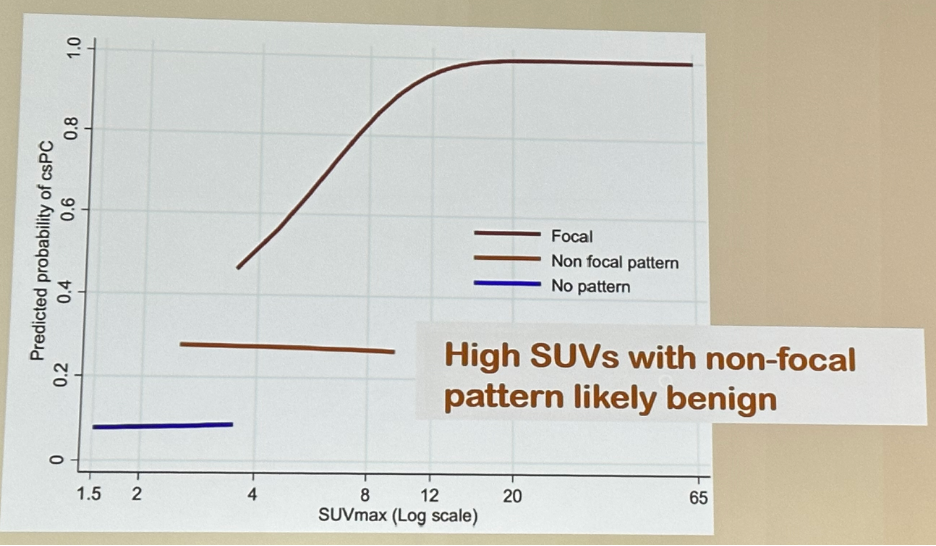
 However, should we rely on SUVmax alone? The SUVmax range of 2.5 to 7.5 is considered the “equivocal” zone for PCa. As such, SUV alone has insufficient accuracy. What appears to be equally important to intensity is actually the pattern of uptake.
However, should we rely on SUVmax alone? The SUVmax range of 2.5 to 7.5 is considered the “equivocal” zone for PCa. As such, SUV alone has insufficient accuracy. What appears to be equally important to intensity is actually the pattern of uptake.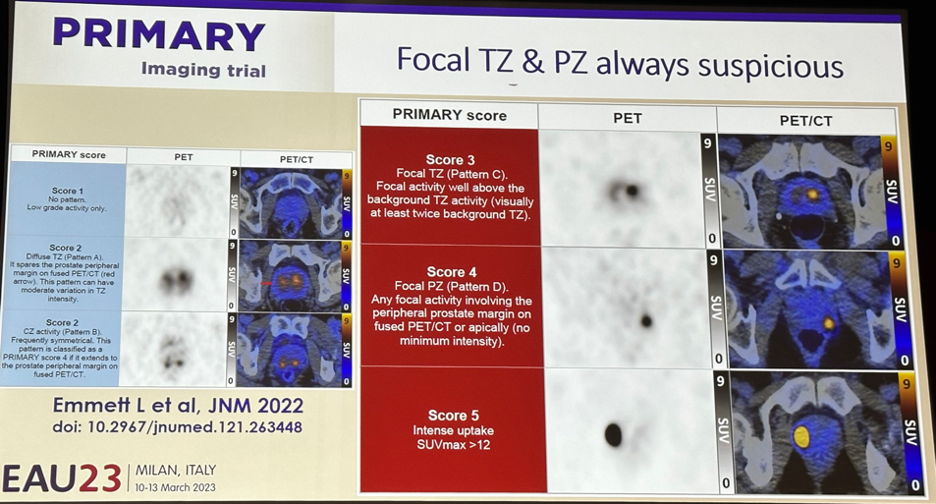
As demonstrated above, the PRIMARY score was derived based on the intensity and pattern of uptake with a 5-point Likert scale analogous to that of the PIRADS for mpMRI. The significance of the pattern of enhancement is highlighted in the figure below. In patients with no or non-focal patterns of uptake, the probability of csPCa plateaus at low levels, irrespective of SUVmax intensity. Conversely, in patients with focal uptake, the predicted probability of csPCa exponentially rises with SUVmax levels.
 Dr. Hofman stressed that we must “beware” PSMA-negative tumors. When csPCa is present, yet not picked up on PSMA-PET, this may actually reflect high grade, poorly differentiated disease without PSMA expression. Fortunately, this was a rare occurrence in the proPSMA study (~2%).
Dr. Hofman stressed that we must “beware” PSMA-negative tumors. When csPCa is present, yet not picked up on PSMA-PET, this may actually reflect high grade, poorly differentiated disease without PSMA expression. Fortunately, this was a rare occurrence in the proPSMA study (~2%). 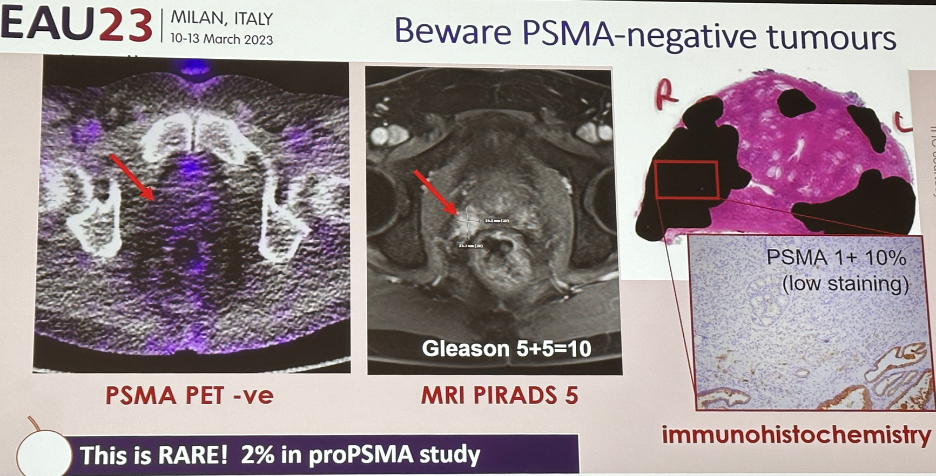
Dr. Hofman next presented the PRIMARY 2 trial protocol, which is a phase III trial evaluating the additive value of PSMA-PET/CT in men with negative or equivocal MRI for diagnosing csPCa. This study will enroll 660 men with MRI PIRADS 2 plus a “red flag” risk factor or PIRADS 3 lesion on mpMRI and randomize patients to “standard of care” template prostate biopsy or a PSMA-PET/CT whereby patients with an abnormal scan undergo a targeted prostate biopsy, whereas those with a negative PET forgo the biopsy.
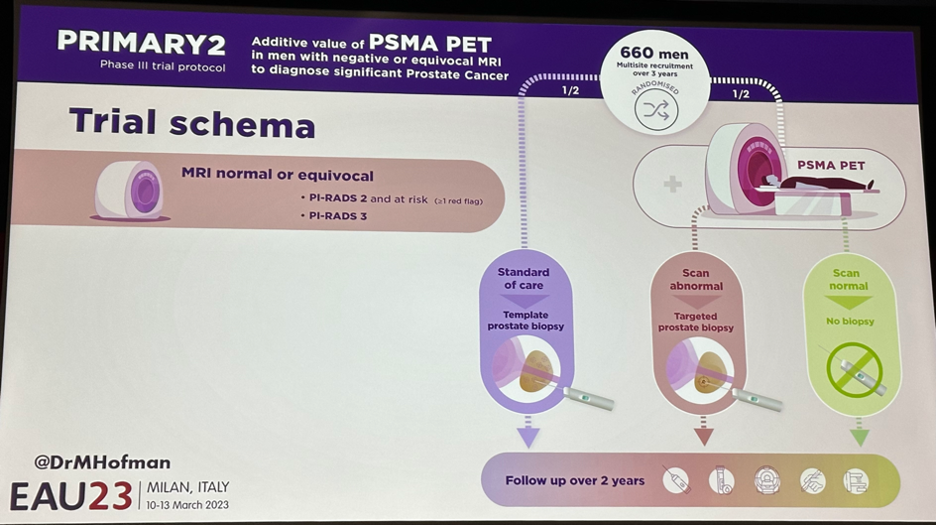
This is a non-inferiority trial evaluating the approach of SOC with MRI alone versus addition of PSMA-PET/CT with avoidance of biopsy in patients with negative findings. One of the objectives is to evaluate complication differences between the 2 arms, secondary to biopsy avoidance in the PET-negative patients. This study will also assess the impact of this approach on health economics and patient reported outcomes (PROs).
In summary, Dr. Hofman concluded that PSMA-PET/CT in the primary setting:
- Allows us to see the invisible tumors that MRI misses
- Allows for a “histopathologic” image with a group of patients that could potentially forgo biopsy
- If intensity is lower, pattern matters: use the PRIMARY score to standardize results
- Should not yet be used for diagnosis. It remains potentially complimentary to mpMRI. We await the PRIMARY2 and other trials in this setting.
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 European Association of Urology (EAU) Annual Meeting, Milan, IT, Fri, Mar 10 – Mon, Mar 13, 2023.
References:
Read the CON Debate: EAU 2023: Case-based debate: Will PSMA PET Supplant Multiparametric MRI for Prostate Cancer Detection? Case Presentation – Con


