When considering the role of metastasis-directed therapy (MDT) in this setting, it is important to distinguish between the terms oligometastasis (a finite number of metastases, often 3 or less) and oligoprogression, an emerging concept in oncology, denoting a state where after an initially successfully systemic therapy of disseminated metastases, a single/few lesions display further progression.
The NCCN guidelines currently endorse the role of MDT (either surgical metastatectomy or SBRT) as a treatment option for patients with relapsed or stage IV clear cell or non-clear cell RCC. The slide below, courtesy of Dr. Amy Luckebaugh at ASCO GU 2023, summarizes the current literature for surgical metastatectomy, which, compared to SBRT, remains an infrequently utilized modality in this disease setting.
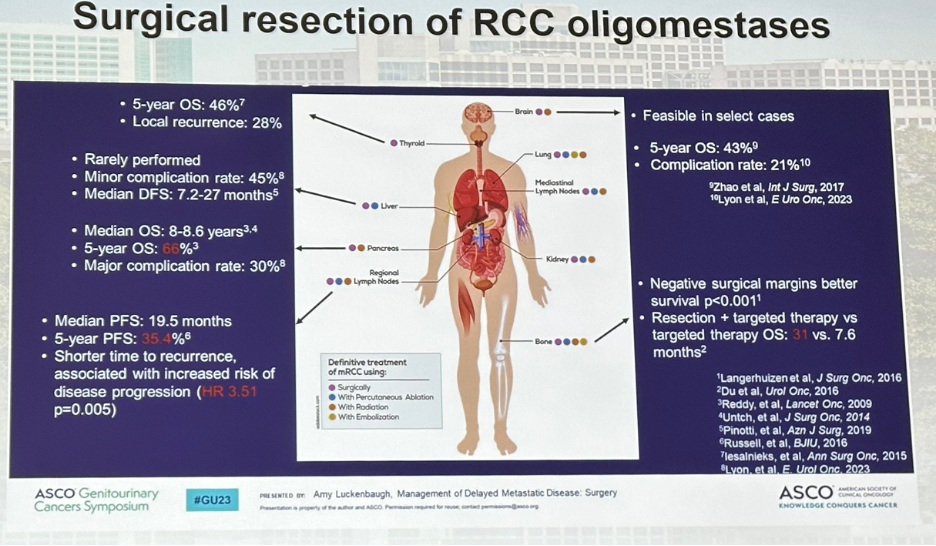 A 2014 systematic review of studies from 2006 to 2011 (TKI, pre-IO era) demonstrated that retrospective series of surgical metastatectomy for RCC have consistently shown overall or cancer-specific survival benefits in favor of metastatectomy.1
A 2014 systematic review of studies from 2006 to 2011 (TKI, pre-IO era) demonstrated that retrospective series of surgical metastatectomy for RCC have consistently shown overall or cancer-specific survival benefits in favor of metastatectomy.1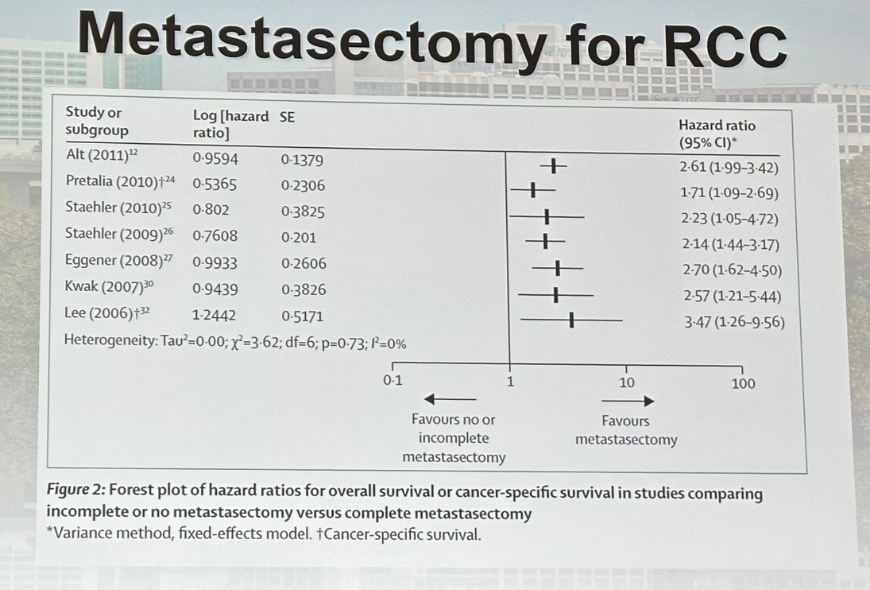 Similar results were observed from a 2019 meta-analysis of studies evaluating SBRT for RCC oligometastases with a pooled 1-year local control rate of 89.1% (95% CI: 84% - 94%). It is important to note however that there is significant heterogeneity between the studies, as is quantified by the reported I2 value of 71%.
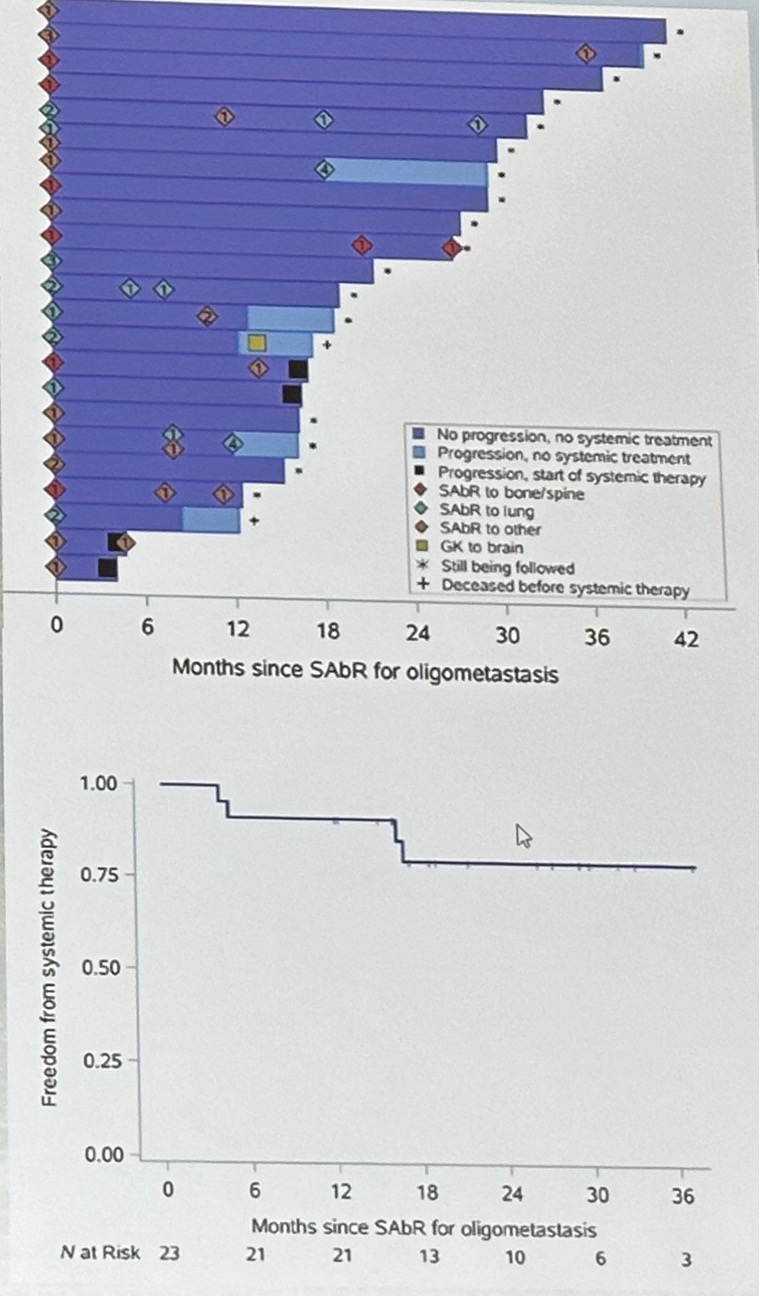
Similar results were observed from a 2019 meta-analysis of studies evaluating SBRT for RCC oligometastases with a pooled 1-year local control rate of 89.1% (95% CI: 84% - 94%). It is important to note however that there is significant heterogeneity between the studies, as is quantified by the reported I2 value of 71%.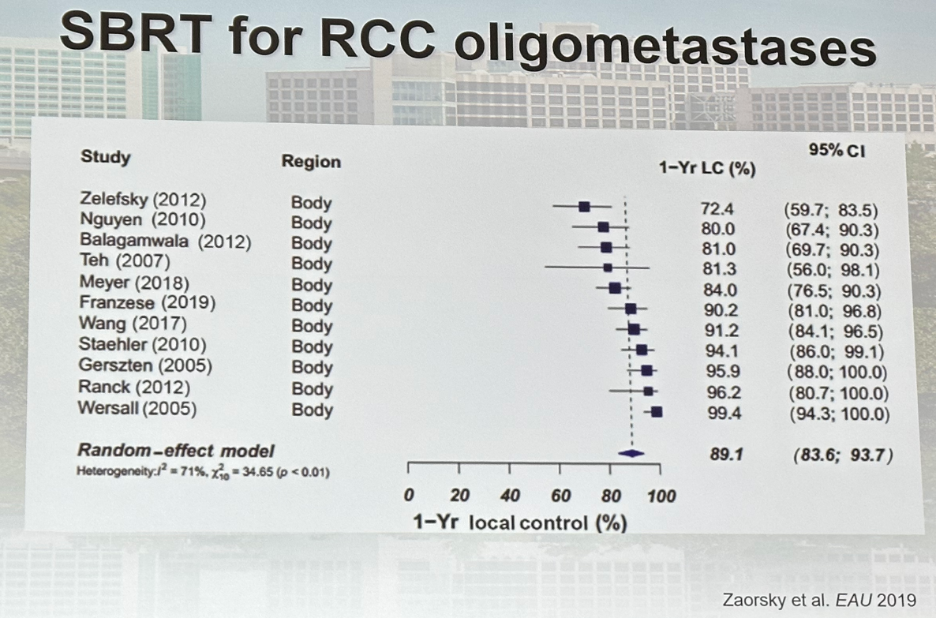 Brugarolas and colleagues recently published the results of a single arm phase II trial that included systemic therapy-naïve patients with oligometastatic disease (3 or less extracranial metastases)3. This cohort included 23 patients with RCC (19 clear cell, 2 papillary, and 2 chromophobe). Patients received sequential SBRT (33 initial and 57 total sites). The primary endpoint was freedom from systemic therapy at 1 year, which was 91.3% (95% CI: 70 – 98%).
Brugarolas and colleagues recently published the results of a single arm phase II trial that included systemic therapy-naïve patients with oligometastatic disease (3 or less extracranial metastases)3. This cohort included 23 patients with RCC (19 clear cell, 2 papillary, and 2 chromophobe). Patients received sequential SBRT (33 initial and 57 total sites). The primary endpoint was freedom from systemic therapy at 1 year, which was 91.3% (95% CI: 70 – 98%).The secondary endpoint results included:
- Local control: 100%
- 1-year PFS: 83%
- Quality of life: unaffected
 A similar phase II trial by Tang et al. evaluated definitive radiotherapy in lieu of systemic therapy for oligometastatic RCC. This single arm phase II feasibility trial included 30 clear cell RCC patients with 5 or less metastases. Up to one previous systemic therapy was permitted (unlike the prior trial which did not allow for prior systemic therapy). Patients received sequential SBRT (or hypofractionated IMRT). The co-primary endpoints were feasibility and PFS. This treatment was noted to be feasible/well-tolerated, with a median PFS of 22.7 months (95%10.4 months – not reached).
A similar phase II trial by Tang et al. evaluated definitive radiotherapy in lieu of systemic therapy for oligometastatic RCC. This single arm phase II feasibility trial included 30 clear cell RCC patients with 5 or less metastases. Up to one previous systemic therapy was permitted (unlike the prior trial which did not allow for prior systemic therapy). Patients received sequential SBRT (or hypofractionated IMRT). The co-primary endpoints were feasibility and PFS. This treatment was noted to be feasible/well-tolerated, with a median PFS of 22.7 months (95%10.4 months – not reached). 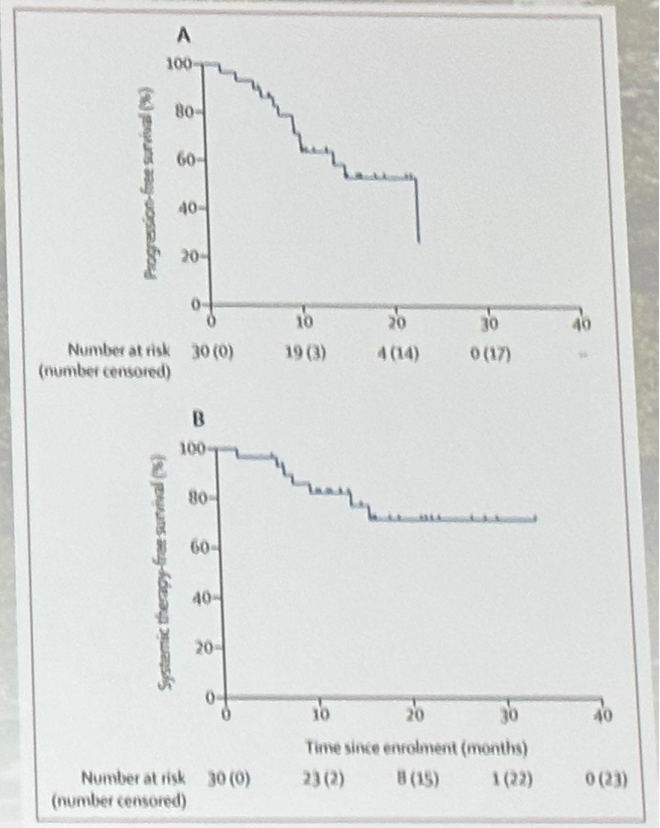 CI:
CI: In contrast to SBRT for oligometastatic RCC, there are currently two published phase II trials of SBRT for oligoprogression as demonstrated below. In the trial by Cheung et al, SBRT was administered to clear cell RCC patients (n=57) on TKI for at least 3 months with prior stability/response and oligoprogression, with a 1-year local control rate of 93% and a median PFS of 9.3 months. The median time from SBRT to therapy change was just over a year. The 1-year OS was 92% and no patient had grade 3-5 SBRT-related toxicities.4 Similar impressive results were seen in the trial by Hannan et al. in 20 patients (both clear and non-clear cell histology) with local control of 100%, SBRT-extended therapy by at least 6 months in 70% of patients, and excellent AE/QoL profile.5
Currently, the parallel arm, phase III SBRT for Oligometastatic Advanced RCC (SOAR) is evaluating sequential SBRT followed by systemic therapy at progression versus systemic therapy only in patients with metastatic RCC with prior surgical resection and IMDC favorable-intermediate risk disease with 2-5 metastatic lesions, all amenable to SBRT.
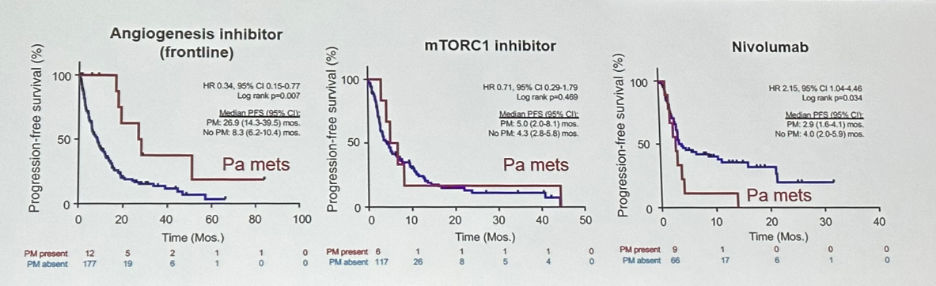 Is there a link between oligometastases and RCC biology? As of yet, this remains poorly understood. Interestingly, about 50% of RCC that metastasize to the pancreas have metastatic lesions isolated to the pancreas. Furthermore, patients with pancreatic metastases appear to have improved overall survival outcomes, which may suggest an underlying biologic/genetic etiology. Studies have suggested that this biologic link is related to PBRM1 loss with prominent angiogenesis and a preferential responsiveness to angiogenesis inhibitors, as demonstrated in the curves below:
Is there a link between oligometastases and RCC biology? As of yet, this remains poorly understood. Interestingly, about 50% of RCC that metastasize to the pancreas have metastatic lesions isolated to the pancreas. Furthermore, patients with pancreatic metastases appear to have improved overall survival outcomes, which may suggest an underlying biologic/genetic etiology. Studies have suggested that this biologic link is related to PBRM1 loss with prominent angiogenesis and a preferential responsiveness to angiogenesis inhibitors, as demonstrated in the curves below: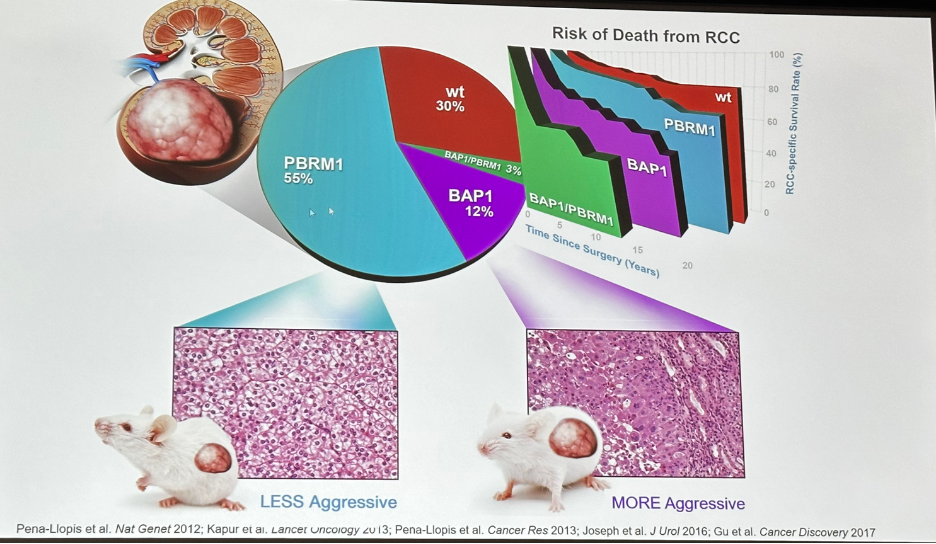 These findings have been confirmed in studies of RCC genetics, whereby patients with PRBM1 loss have an association with low-grade disease. This was confirmed in mouse-based models, whereby mice with PRBM1 induced mutations had the development of less aggressive renal tumors.
These findings have been confirmed in studies of RCC genetics, whereby patients with PRBM1 loss have an association with low-grade disease. This was confirmed in mouse-based models, whereby mice with PRBM1 induced mutations had the development of less aggressive renal tumors.How does one integrate MDT and systemic treatment in patients with oligometastatic RCC? Dr. Brugarolas noted the following to consider:
- Thorough evaluation of the extent of metastatic disease: location, number, and size of all metastases
- Patient’s overall health, comorbidities, and life expectancy
- The aim of MDT should be to eradicate all visible metastases while preserving organ function, minimizing toxicity and improving OS
- To this end he highlighted a case from his clinical practice, whereby a patient with centrally-located pulmonary metastases treated with SBRT experienced life-threatening hemoptysis
- The biology/pace of the disease
- A period of active surveillance may be appropriate
- The choice of treatment will depend on factors such as the location and size of the metastases, the patient’s overall health, timing of metastases, and the experience of the treating team
- Interventions may be repeated over time while the disease remains oligometastatic
- James Brugarolas, MD, PhD, Director of the Kidney Cancer Program, Harold C. Simmons Comprehensive Cancer Center, The Sherry Wigley Crow Cancer Research Endowed Chair in Honor of Robert
- Lewis Kirby, M.D., UT Southwestern Medical Center, Dallas, TX
References:
- Dabestani et al. Lancet Oncol 2014.
- Zaorsky et al. Eur Urol 2022.
- Hannan et al. Eur Urol Oncol 2022.
- Cheung et al. Eur Urol 2021.
- Hannan et al. Eur Urol Oncol 2022.


