(UroToday.com) The 2023 European Association of Urology (EAU) annual congress held in Milan, Italy between March 10th and 13th, 2023 was host to a rapid-fire debates session addressing common problems and controversies in bladder cancer, chaired by Dr. Ashish Kamat. Following a case presentation by Dr. Jørgen Bjerggaard Jensen, Dr. Param Mariappan was tasked with debating against prostate-sparing radical cystectomy in men and reproductive organ-sparing in women as safe options for patients with muscle-invasive bladder cancer. Conversely, Dr. Maria Carmin Mir was tasked with debating in favor of such approaches.
Dr. Jensen began by presenting the case of a 42-year-old male who presented with hematuria. This patient was otherwise healthy with a body mass index of 23 kg/m2. At the time of presentation, the patient denied any lower urinary tract symptoms, had no erectile dysfunction, and a PSA of 0.5 ng/ ml (MRI was thus not obtained). He was noted on cystoscopy to have a 1.5 cm tumor in the dome of the bladder, and a subsequent TURBT demonstrated pure urothelial T2 disease without CIS in the bladder or prostatic urethra. In accordance with local institutional protocols, the patient received four cycles of neoadjuvant gemcitabine and cisplatin. Of note, the patient has a wife in her thirties, and they had not yet completed planned childbearing at the time of presentation.
The second case was that of a 32-year-old female also with no prior medical history and a body mass index of 21 kg/m2. She was found to have a 5 cm pure urothelial T3 tumor located along the left bladder wall, above the ureteric orifice and not involving the trigone. No CIS was present in the specimen. On manual examination, the tumor was palpable, but mobile and not involving the vagina. The patient’s only complaint was urgency in the weeks leading up to the diagnosis and following the TURBT. The patient was offered neoadjuvant chemotherapy with gemcitabine/cisplatin and offered nivolumab if she did not want neoadjuvant chemotherapy, only if T3 or N+ disease was present following surgery. This patient is married to patient 1 and is also planning on having kids within the next few years.
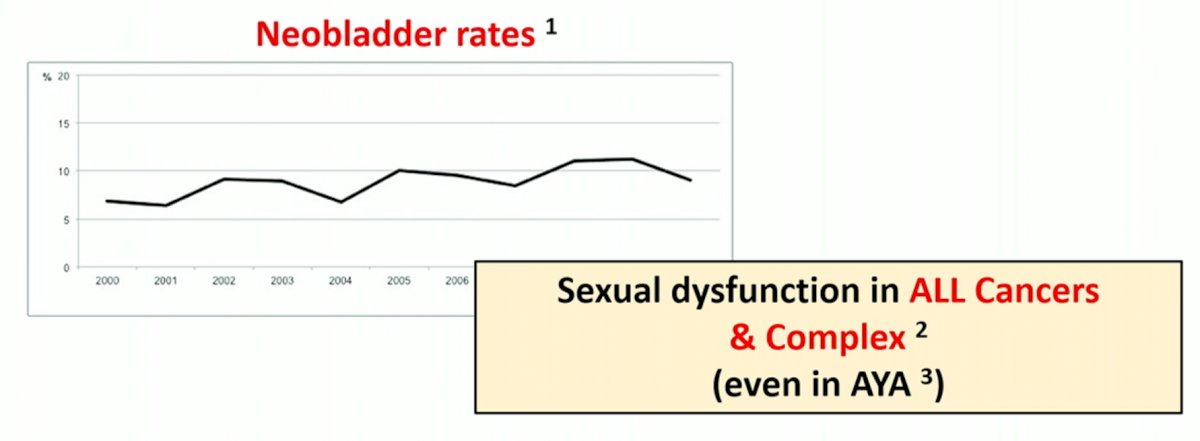
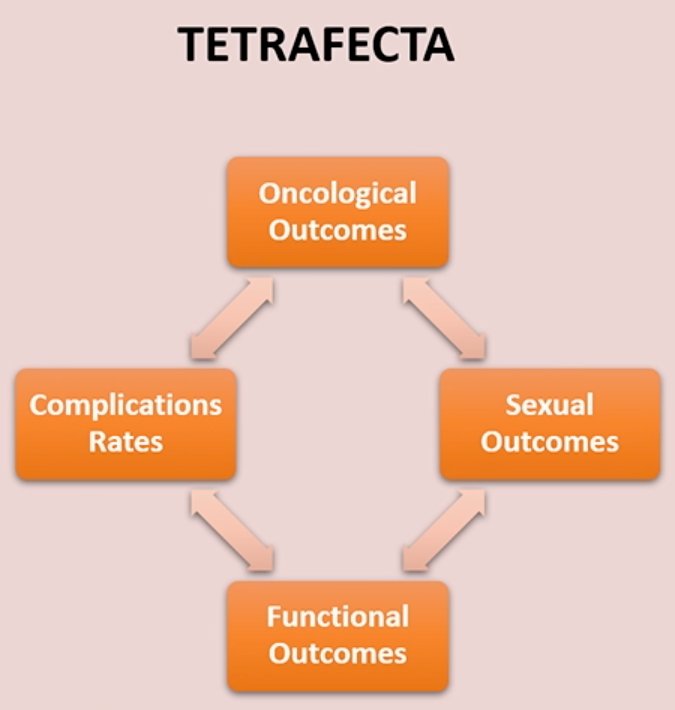
Dr. Mariappan began the debate by acknowledging that the rationale of reproductive organ-sparing surgery is to preserve continence and sexual function, without compromising oncologic outcomes in well-selected patients. He argues however that we have not done a good job as urologists in adopting measures that could potentially improve patient continence and sexual function. Neobladders are a form of a continent diversion, and, as such, offer the advantage of ‘controlled’ continence when compared to ileal conduits. However, neobladder adoption rates have hovered around 10%, which is a disappointing figure, even when accounting for patient-related factors precluding neobladder creation, such as poor renal function and poor manual dexterity. Furthermore, the risk of sexual dysfunction is increased in all patients with malignancy and may be inherent to the stress secondary to the diagnosis of malignancy.
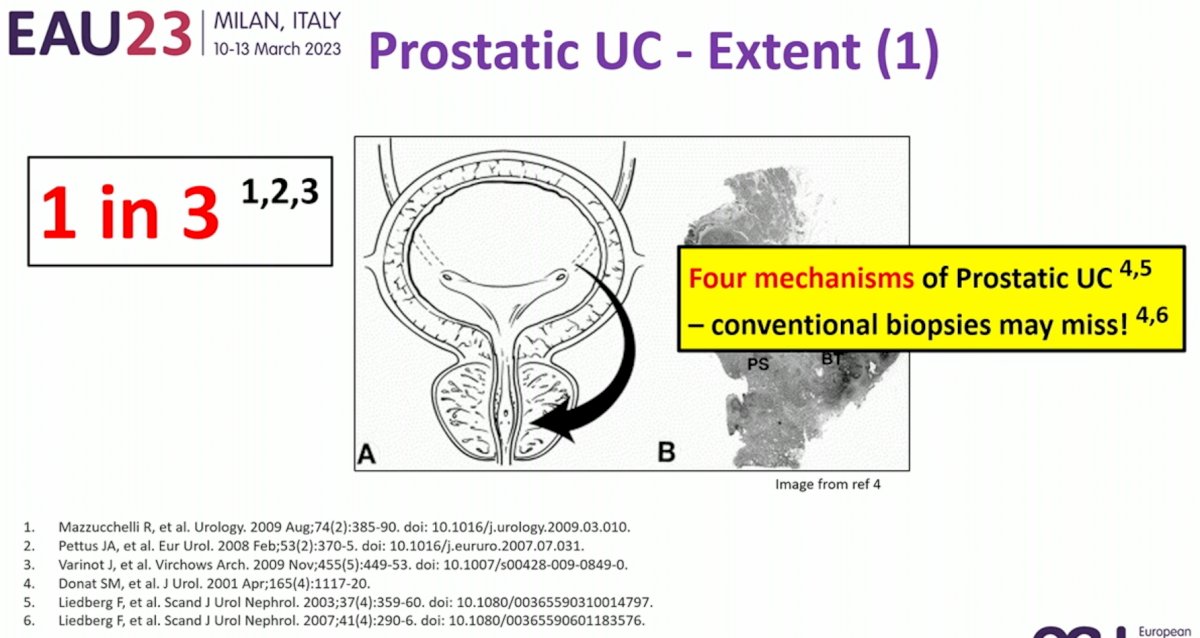
What are the practical challenges to widespread adoption of reproductive organ sparing? These can be summarized using the acronym C-I-S: clearance, information, and safety. With regards to clearance, we need to be confident that we are clearing (i.e. not missing) a concurrent diagnosis of prostate cancer or prostatic urothelial malignancy. In some MIBC patient cohorts, up to 1 in 3 patients have a concurrent diagnosis of prostatic urothelial carcinoma and conventional biopsies may miss this malignancy.
One may argue that appropriate patient selection (e.g. no multifocal cancer, no trigone/bladder neck cancer, no CIS) may reduce this risk and make reproductive organ-sparing cystectomy feasible. However, Dr. Mariappan argued that this logic may be flawed due to limitations of current diagnostic procedures with missed visible tumor in 14-64% of repeat TURBT procedures.1 Furthermore, such missed non-visible tumor may be CIS in etiology, which has important prognostic implications, particularly with regards to ‘field cancerization’.

With regards to Information (“I” in CIS), we know that the risk of upstaging at time of RC is significant, and this has important implication for worse cancer-specific survival.2 Furthermore, such patients with disease upstaging are at increased risk of reproductive organ involvement.

Another complicating factor is that variant histology, a potential surrogate of advanced cancer and reproductive organ involvement, is missed in over 40% of cases in some series.3
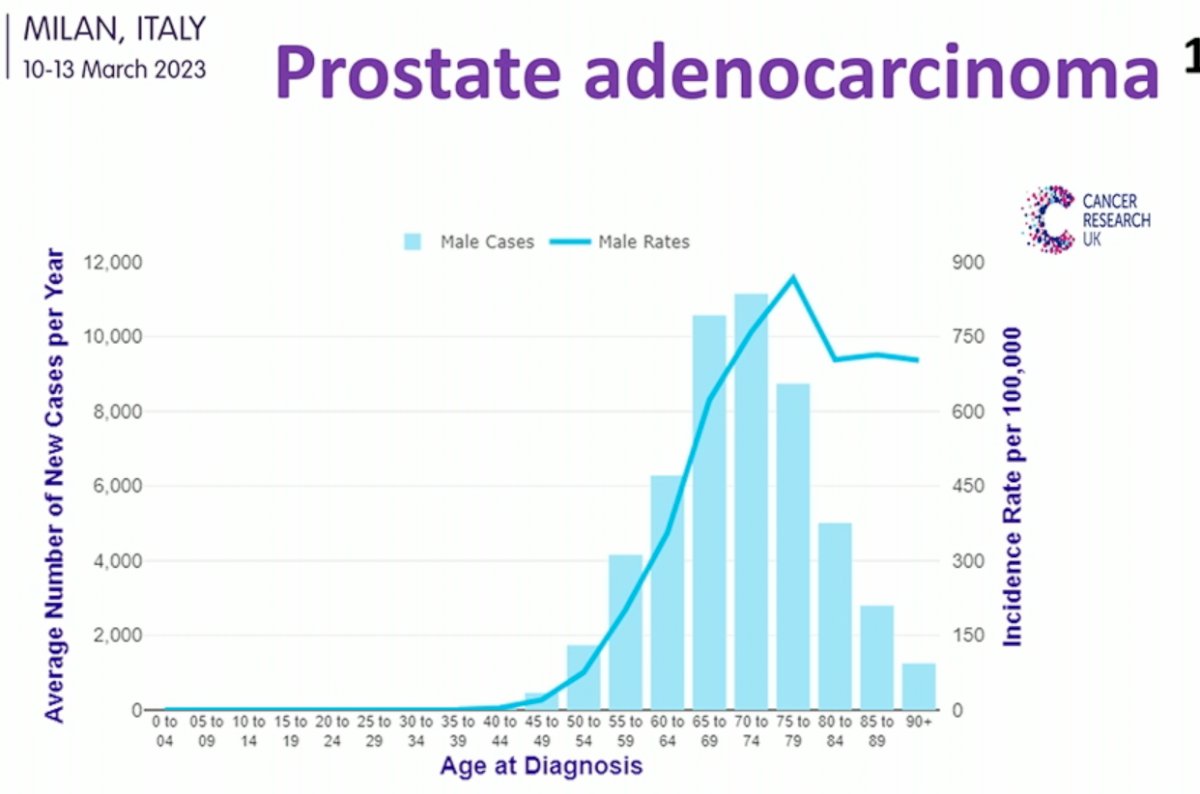
With regards to safety (“S” component in CIS), Dr. Mariappan addressed concerns regarding future cancer developing in the preserved organs. The incidence of prostate cancer increases significantly as patients age, with approximately 1 in 7 to 8 males diagnosed during their lifetime.
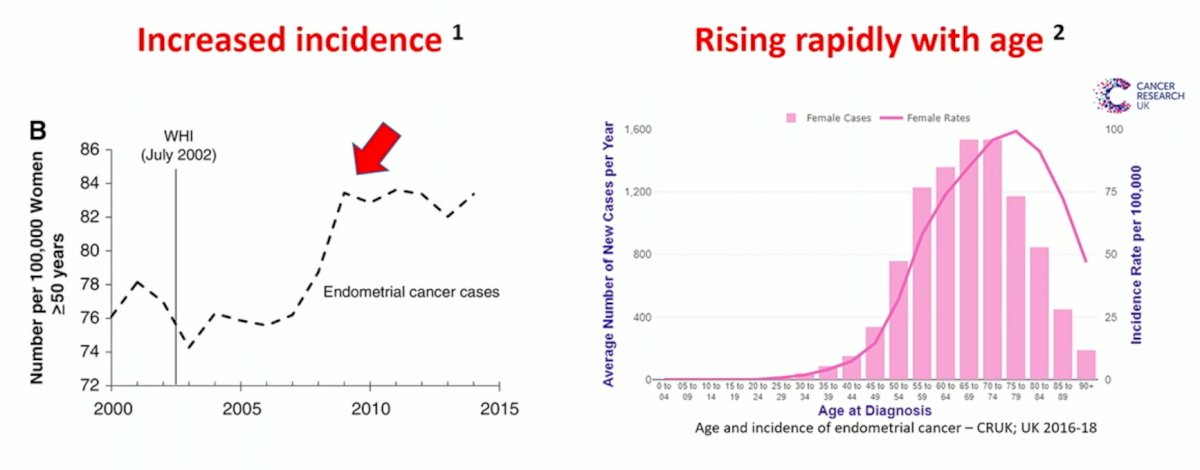
What about malignancy in the female reproductive organs? The incidence of endometrial malignancy has significantly increased over the last decade and, similar to prostate cancer, rapidly rises with age.
Furthermore, as most ovarian cancer actually arises from the cellular lining of the inner fallopian tubes, the American College of Obstetricians and Gynecologists (ACOG) recommends opportunistic salpingectomy to reduce the incidence of ovarian cancer.

Readdressing the issue of incontinence – it is postulated that reproductive organ sparing may improve incontinence, however all studies suggesting that there is an association between such organ sparing surgeries and improved continence are limited by small sample sizes and non-randomized comparisons with an associated high risk of bias. With regards to sexual dysfunction, managing this issue remains complex and is not simply fixed by organ preservation. As such, Dr. Mariappan concluded that as surgeons we face a tough-balancing act in this situation: how do we balance surgical aggression with reproductive organ preservation?
At this point, the debate was turned over to Dr. Mir to argue in favor of reproductive organ sparing in this situation. She began by acknowledging that a prostate-sparing RC remains controversial, and the current EAU guidelines do not recommend such approaches. There are however nuances to such an approach that are not restricted to prostate-sparing surgery only. Patients can undergo capsule sparing, seminal sparing, and nerve-sparing RCs, all of which have the theoretical advantages of improved continence and sexual functions.
For the patient in question, Dr. Mir is of the opinion that he fits all requisite criteria for prostate-sparing RC:
- He has cT2 or less disease
- He is young
- He has a good performance status
- He has had a negative TUR/biopsy of the prostatic urethra and bladder neck
- His PSA is <4 ng/ml with no evidence of an abnormal rectal exam (MRI/biopsy not indicated given his PSA)
- He has excellent preoperative sexual function and continence
Furthermore, he wants to maintain childbearing ability and thus will need sperm banking prior to neoadjuvant chemotherapy (adversely affects spermatogenesis) and surgery (high risk of ejaculatory dysfunction).
In 2015, Jacobs et al. published the results of small (n=40) parallel arm RCT comparing prostate-sparing to nerve-sparing radical cystectomy. As demonstrated below, there were no differences in the functional urinary or sexual outcomes, with oncologic equivalency demonstrated.4 Notably, patients in the nerve-sparing cystectomy arm had a significantly higher rate of Clavien-Dindo 3 or worse complication rate within 90 days of surgery (60% versus 35%), However, Dr. Mir argues that this study was underpowered to evaluate for differences in these functional outcomes.

A study by Saad et al. published in 2019 demonstrated that patients undergoing a prostate-sparing RC had superior functional outcomes to those undergoing a nerve-sparing RC. At 3 months, both daytime and nighttime incontinence were better in the prostate-sparing arm. Sexual function, defined as potency with no treatment required, at 12 months was present in 53% of patients in the prostate-sparing cohort, compared to 9% in the nerve-sparing cohort. Oncologic outcomes were non-significantly different (90% versus 78%) and major complications were also similar (13% versus 20%).
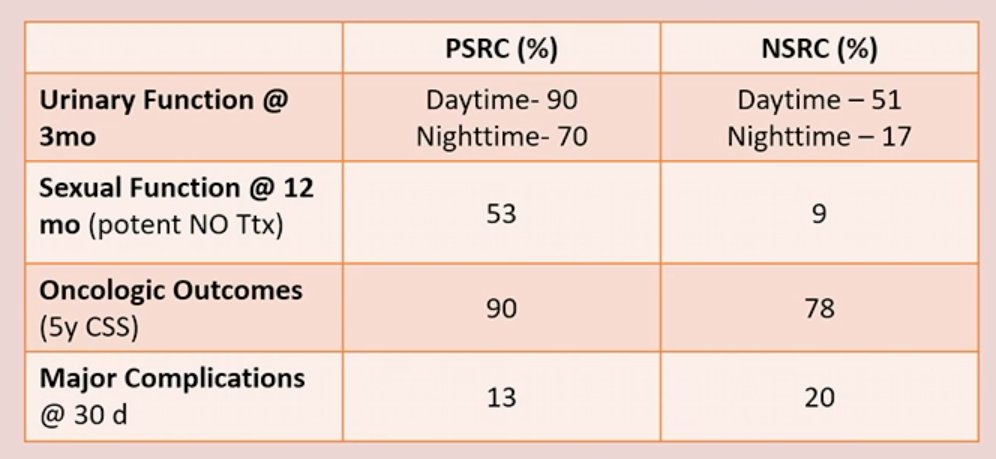
Similar to Dr. Mariappan beforehand, Dr. Mir acknowledged that there are oncologic risks associated with prostate-sparing RC. Urothelial recurrence adversely affects overall survival. Prostatic urethral recurrence is a valid concern with a 20% failure rate for transurethral biopsies and concerns about positive surgical margin rates (~7%). Furthermore, there is a 20% incidence of csPCa in prostates removed during RC. As such, we should be weary of such risks and patient selection remains key to minimizing adverse oncologic outcomes.
What about stigmas ascribed to female RCs? Females are known to have worse outcomes after RC. There is often a delay in treatment secondary to delayed hematuria work ups, potential hormonal effects potentiating worse host biology, and worse overall survival outcomes. In the case presented, Dr. Mir argued that female organ sparing RC may improve daytime continence rates, improve vaginal lubrication and thus decrease dyspareunia, and better preserve the ability to achieve an orgasm. The cons are potentially an increased risk of urethral and vaginal wall recurrences.
She also addressed concerns about not performing an ‘opportunistic’ oophorectomy/salpingectomy as recommended by the ACOG. While the advantages to performing this include:
- Eliminating the risk of ovarian cancer, which is particularly pertinent given that screening is not feasible, and this is the gynecologic malignancy with the highest death rate
- Decreased risk of breast cancer
- Eliminates the risk of bladder cancer involving the ovaries
She argued that disadvantages are also common, and include:
- An increased risk of:
- Mortality
- Cardiac disease
- Stroke
- Osteoporosis
- Hip fracture
- Cognitive impairment
- Iatrogenic menopause in younger patients
- Development of sexual dysfunction

What about the oncologic safety of female reproductive organ-sparing cystectomy? A comparative analysis by Patel et al. published in 2022 demonstrated that this approach is safe and effective in women with variant histology and advanced stage.5

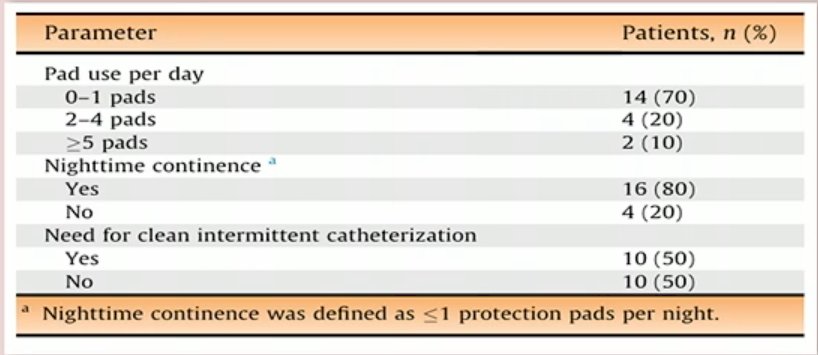
Recent evidence has also emerged that the functional benefits of such an approach in females extend to the robotic cystectomy literature as well as demonstrated below:
Dr. Mir concluded her presentation by summarizing the following key requirements prior to considering pelvic organ sparing RC in MIBC patients:
- A motivated patient
- A sexually active patient who wants to preserve sexual function
- A patients with localize MIBC
- A patient that understands the risk of disease recurrence and upstaging
Further considerations in this space include:
- Does this cohort of patients overlap with those that could potentially benefit from bladder-sparing approaches (i.e. trimodality therapy)?
- Functional and oncologic outcomes need to be further evaluated with MIS techniques
- Bladder MRI may be helpful for surgical planning and addressing upstaging concerns
- Molecular markers in this space may assist with appropriate patient selection
- Dr. Param Mariappan, MBBS (Hons), FRCS (Urol), FRCSEd, FEBU, Consultant Urological Surgeon and Honorary Clinical Senior Lecturer · Western General Hospital, Edinburgh; University of Edinburgh; Spire Murrayfield Hospital, Edinburgh, Scotland
- Dr. Maria Carmen Mir, MD, PhD, FEBU, Department of Urology, Fundacion Instituto Valenciano Oncologia, Valencia, Spain
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 European Association of Urology (EAU) Annual Meeting, Milan, IT, Fri, Mar 10 – Mon, Mar 13, 2023.
References:- Cumberbtach, et al. Repeat Transurethral Resection in Non-muscle-invasive Bladder Cancer: A Systematic Review. Eur Urol 2018. (6):925-933
- Shariat, et al. Discrepancy between clinical and pathologic stage: impact on prognosis after radical cystectomy. Eur Urol 2007. 51(1):137-49.
- Shah, et al. Variant (divergent) histologic differentiation in urothelial carcinoma is under-recognized in community practice: impact of mandatory central pathology review at a large referral hospital. Urol Oncol 2013. 31(8):1650-5.
- Jacobs, et al. Prostate capsule sparing versus nerve sparing radical cystectomy for bladder cancer: results of a randomized, controlled trial. J Urol 2015. 193(1):64-70.
- Patel, et al. Estimated Indirect Cost Savings of Using Telehealth Among Nonelderly Patients With Cancer. Clinic GU 2022. 6(1):e2250211.
Pros and Cons of Organ-Sparing Cystectomy in Bladder Cancer Patients: Balancing Oncologic and Functional Outcomes - Param Mariappan & Maria Carmen Mir


