UroToday.com) The 2023 EAU annual meeting included a rapid fire session discussing common problems and controversies in bladder cancer, featuring a debate assessing the best transurethral resection strategy.
Case Presentation
Dr. J. Alfred Witjes started with a case presentation of an 84 year old male with a treatment history as follows:
- 2008: pT1HG and CIS treated with 3 years of BCG
- 2012: pT2G2 treated with mitomycin C, followed by epirubicin because he developed a mitomycin C allergy
- 2017/2018: repeatedly developed CIS and underwent several induction courses of BCG and eventually was sent to Nijmegen for chemohyperthermia (Synergo)
- February 2019: started Synergo, and biopsies in July 2019 were negative
- December 2021: cytology showed TPS2, cystoscopy was normal, however he stopped Synergo
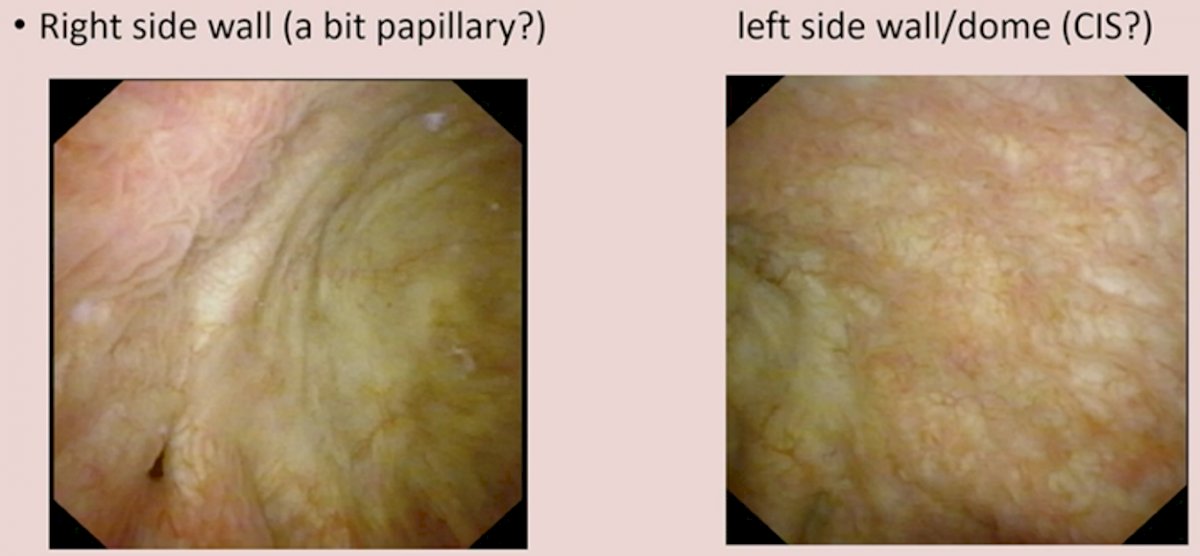
- January 2023: CT urogram was negative for upper tract disease, cytology went from TPS2 to TPS4, and EpiCheck was 87 (normal <60). Cystoscopy showed:
 PDD/NBI is Useful and Benefits Patients
PDD/NBI is Useful and Benefits Patients
The position of PDD/NBI being useful for patients was taken by Dr. Marek Babjuk. He notes that in a 2013 meta-analysis assessing the available clinical data for blue light hexaminolevulinate cystoscopy on the detection of Ta/T1 and CIS tumors, Burger et al.1 found that blue cystoscopy detected significantly more Ta tumors (14.7%; p<0.001; OR 4.90, 95% CI, 1.94-12.39) and CIS lesions (40.8%; p<0.001; OR 12.37, 95% CI, 6.34-24.13) than white light. There were 24.9% patients with at least one additional Ta/T1 tumor seen with blue light (p<0.001), significant also in patients with primary (20.7%; p<0.001) and recurrent cancer (27.7%; p<0.001), and in patients at high risk (27.0%; p<0.001) and intermediate risk (35.7%; p=0.004) disease. In 26.7% of patients, CIS was detected only by blue light (p<0.001) and was also significant in patients with primary (28.0%; p<0.001) and recurrent cancer (25.0%; p<0.001).
As such, Dr. Babjuk suggests that blue light can likely improve detection of tumors, however can advanced imaging also improve completeness of TURB? The BRIGHT study prospectively registered high-risk non-muscle invasive bladder cancer patients with an initial photodynamic diagnosis (PDD) - transurethral resection of bladder tumor (n = 177).2 These patients were then compared to high-risk non-muscle invasive bladder cancer cases with a history of initial white-light transurethral resection of bladder tumor (n = 306). This study found that the residual tumor rates in the photodynamic diagnosis group was 25.7% and in the white-light group was 47.3%. Dr. Babjuk notes that yes, perhaps advanced imaging can improve completeness of TURBT.
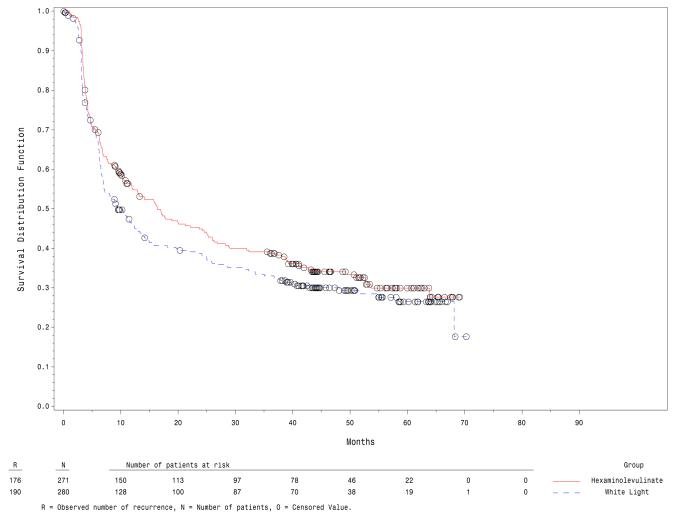
Can the advantages of advanced imaging alter the natural history of the tumor? Are improvements in detection ultimately translated to better outcomes? In 2012, Grossman and colleagues assessed the impact of hexaminolevulinate fluorescence cystoscopic detection of papillary, non-muscle invasive bladder cancer on the long-term recurrence rate.3 Among 280 patients in the white light group and 255 in the fluorescence group, over a median follow-up of 53.0 and 55.1 months, respectively, 31.8% in the white light group and 38% in the blue light group remained tumor free. Median time to recurrence was 9.4 months in the white light group and 16.4 months in the fluorescence group (p = 0.04):
In a subsequent Cochrane review of 1,847 patients, narrow band imaging (NBI) + white light cystoscopy TURBT was suggested to perhaps lower the risk of disease recurrence, however with a rating of “limited confidence.” The question is which patients may this technology have the most benefit? Work from Dr. Babjuk’s group suggests that 5-aminolaevulinic acid-induced fluorescence cystoscopy during TUR reduces the recurrence rate in stage Ta/T1 bladder cancer, with the most significant benefit in patients with multiple and recurrent tumours.5
Standard TUR is Sufficient, Additional Gimmicks are not Needed
The position of standard TUR is sufficient was taken by Dr. Joan Palou who notes that cystoscopy is an important step in the diagnosis and management of patients with bladder cancer. Additionally, quality of the cystoscopy is completely operator dependent, and tumor detection rate with cystoscopy improves with the awareness of positive urine tests. A recently published randomized trial from Gallioli and colleagues [5] compared TURBT and en-bloc resection of bladder tumor in pathological diagnosis, surgical, and oncological outcomes. This study enrolled 300 patients diagnosed with bladder cancer and undergoing endoscopic intervention. Inclusion criteria were: tumor size of ≤3 cm, and ≤3 lesions, and no sign of muscle invasion and/or ureteral involvement. The primary outcome is the staging of bladder cancer. Ultimately, 108 (43.5%) and 140 (56.5%) patients were submitted to TURBT and en-bloc resection of bladder tumor, respectively. The rate of Tx disease was comparable (2.8% TURBT vs 4.3% en-bloc resection of bladder tumor). T1 substaging was feasible in 80% TURBT vs 100% en-bloc resection of bladder tumor (p=0.02). Over a median follow-up was 15 months (IQR 7-28), the 3 month recurrence rate was 0% for TURBT and 0.7% for en-bloc resection of bladder tumor (p = 1.0). The overall recurrence rate was 17.6% for TURBT versus 12.9% for en-bloc resection of bladder tumor (p = 0.3).
In a study from Dr. Palou’s group [6] published in 2012, they evaluated the rate of residual tumor and understaging in patients with high grade non-muscle-invasive bladder cancer who underwent second transurethral resection. Among 47 patients, 22 underwent a second TUR because of the absence of muscle in the initial resection specimen (cTx). There was residual disease in 8/47 patients (17%) and understaging in 2 cases (4.2%), the only 2 patients understaged muscularis propria was not present in the sample of initial TUR. The other 20 cTx (90%) patients were cT0 in the re-TUR.
In a study from Dr. Palou’s institution published in 2015,7 they sought to assess the sensitivity and specificity of blue-light cystoscopy with hexaminolevulinate as an adjunct to white-light cystoscopy vs white-light cystoscopy alone for the detection of non-muscle-invasive bladder cancer, in routine clinical practice in Spain. Overall, they detected 1,569 lesions among 283 patients: 621 were tumor lesions according to histology and 948 were false-positives. Among the 621 tumor lesions, 475 were detected by white-light cystoscopy (sensitivity 76.5%, 95% CI 73.2-79.8) and 579 were detected by blue-light cystoscopy (sensitivity 93.2%, 95% CI 91.0-95.1; p < 0.001).
Dr. Palou notes that perhaps the biggest indictment against photodynamic therapy is the recently presented and published results of the PHOTOdynamic trial.8 This was a pragmatic, open-label, parallel-group randomized trial conducted in 22 UK hospitals (n=538), with a suspected first diagnosis of NMIBC at intermediate or high risk for recurrence on the basis of routine visual assessment before being listed for TURBT. Participants were assigned (1:1) to PDD-guided TURBT or to standard white light–guided TURBT. The primary clinical outcome was time to recurrence at 3 years of follow-up, analyzed by modified intention to treat. After a 44 month median follow-up, 86 of 209 in the PDD group and 84 of 217 in the white-light group had recurrences. The hazard ratio for recurrence was 0.94 (95% CI, 0.69 to 1.28; p=0.70):

Dr. Palou finished his presentation by noting several points from the EAU guidelines:
- Take biopsies from abnormal looking urothelium. Biopsies from normal-looking mucosa (mapping biopsies) are recommended if cytology or a urinary molecular marker test is positive. If the equipment is available, perform fluorescence-guided biopsies (strength rating: strong)
- Take a biopsy of the prostatic urethra in cases of bladder neck tumor, if bladder carcinoma in situ is present or suspected, if there is a positive cytology or urinary molecular marker test without evidence of tumor in the bladder, or if abnormalities of the prostatic urethra are visible. If biopsy is not performed during the initial procedure, it should be completed at the time of the second resection (strength rating: strong)
Dr. Palou concluded his presentation with the following take home messages:
- Have a good look at the bladder and take your time
- Do a first good TURBT
- In high grade tumors, white light cystoscopy is doing very well
Case Presented by: J. Alfred Witjes, MD, PhD, Radboud University Nijmegen, The Netherlands
Debater 1: Marek Babjuk, MD, PhD, Charles University and Motol University Hospital, Prague, Czech Republic
Debater 2: Joan Palou, MD, PhD, FEBU, FRCS (Glas), Autonomous University of Barcelona, Barcelona, Spain
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 European Association of Urology (EAU) Annual Meeting, Milan, IT, Fri, Mar 10 – Mon, Mar 13, 2023.
References:
- Burger M, Grossman HB, Droller M, et al. Photodynamic diagnosis of non-muscle-invasive bladder cancer with hexaminolevulinate cystoscopy: A meta-analysis of detection and recurrence based on raw data. Eur Urol. 2013 Nov;64(5):846-854.
- Kobayashi K, Matsuyama H, Kawai T, et al. Bladder cancer prospective cohort study on high-risk non-muscle invasive bladder cancer after photodynamic diagnosis-assisted transurethral resection of the bladder tumor (BRIGHT study). Int J Urol. 2022 Ju;29(7):632-638.
- Grossman HB, Stenzl A, Fradet Y, et al. Long-term decrease in bladder cancer recurrence with hexaminolevulinate enabled fluorescence cystoscopy. J Urol. 2012 Jul;188(1):58-62.
- Babjuk M, Soukup V, Petrik R, et al. 5-aminolaevulinic acid-induced fluorescence cystoscopy during transurethral resection reduces the risk of recurrence in stage Ta/T1 bladder cancer. BJU Int 2005 Oct;96(6):798-802.
- Gallioli A, Diana P, Fontana M, et al. En bloc versus conventional transurethral resection of bladder tumors: A single-center prospective randomized noninferiority trial. Eur Urol Oncol. 2022 Aug;5(4):440-448.
- Gaya JM, Palou J, Cosentino M, et al. A second transurethral resection could be not necessary in all high grade non-muscle-invasive bladder tumors. Actas Urol Esp 2012 Oct;36(9):539-544.
- Palou J, Hernandez C, Solsona E, et al. Effectiveness of hexaminolevulinate fluorescence cystoscopy for the diagnosis of non-muscle invasive bladder cancer in daily clinical practice: A Spanish multicentre observational study. BJU Int 2015 Jul;116(1):37-43.
- Heer R, Lewis R, Vadiveloo T, et al. A randomized trial of PHOTOdynamic Surgery in Non-Muscle-Invasive Bladder Cancer. NEJM Evid 2022;1(10).


