Lynch Syndrome is a common genetic syndrome and the first hereditary cancer-prone syndrome to be identified. 1 in 250-1000 individuals have Lynch Syndrome – and it accounts for 1-4% of all colorectal cancers! However, it is an underappreciated cause of UTUC – and possibly other urologic cancers. What we know about this disease and its implications on GU malignancies is just the tip of the iceberg.
There are 2 different clinical criteria currently used to screen and identify potential Lynch syndrome patients.
The first is the Amsterdam II criteria (1999):
- 3 or more family members (one of whom is a 1st degree relative of the other two) with Lynch syndrome-related cancers
- Two successively affected generations
- One or more colon cancers diagnosed before age 50
Revised Bethesda Criteria (2003):
- Colorectal cancer diagnosed at an age < 50 years
- Presence of synchronous or metachronous colon cancer or another Lynch Syndrome associated malignancy
- Colorectal cancer with MSI-high pathologic associated features
- Lynch Syndrome diagnosed with at least 1 1st degree relative younger than 50 years
- Patient with colorectal cancer orLynch Syndrome associated tumor at any age in 2 first or second degree relatives
If clinical criteria fail, immunohistochemistry is the best current options (sens/spec 83 and 89%, respectively). IHC tests tumor tissue for lack of mismatch repair genes (MMR genes) that are pathognomonic for Lynch Syndrome – MSH 2, MSH 6, MLH1 and PMS2.
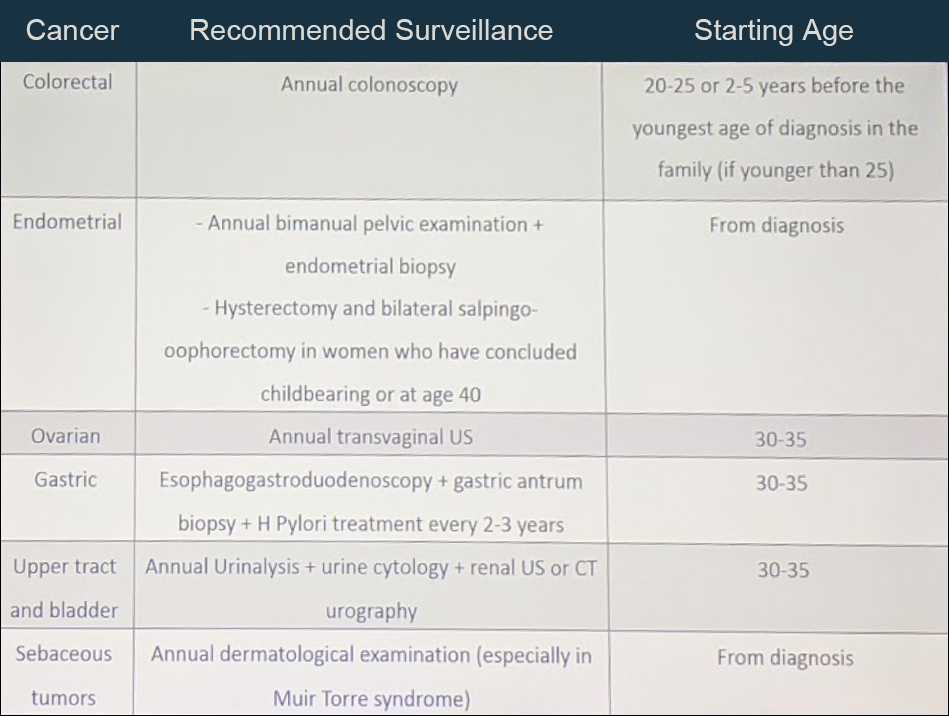
Once diagnosed with Lynch Syndrome, patients have stringent protocols to diagnose other Lynch Syndrome-associated malignancies earlier – as they often present with earlier, aggressive tumors (especially colon cancer). Below is a recommended surveillance strategy for LS mutation carriers:
Looking now, specifically at Lynch Syndrome and UTUC:
- Lynch Syndrome increases risk of UTUC 4-17 times for renal UTUC and 8-12 times for ureteral UTUC
- MSH2 mutation carriers carry an even higher risk of UTUC compared to MLH1 carriers
- Of the Lynch Syndrome-associated tumors, UTUC is the 3rd most common! Reported lifetime risk is 3-28%
- A proportion of hereditary of UTUC is probably being misclassified at sporadic currently – and these patients are missing the opportunity to be screened for Lynch Syndrome-associated malignancies
- Lynch Syndrome-associated UTUC
- More common among women
- Diagnosed at younger ages (~62 years vs. 70 for sporadic UTUC)
- Higher proportion of ureteral tumors (51%)
- Higher risk of developing bilateral tumors
- Better response rates to adjuvant chemotherapy (due to mismatch repair)

Important that you send patients with suspected Lynch Syndrome to a genetic counselor, so they can complete cascade testing of family members and set up appropriate screening
As for screening for UTUC in Lynch Syndrome patients, a 2015 panel of experts recommended the following:
- Yearly urinalysis with a threshold of 3 RBC/hpf for evaluation with cystoscopy
- CT Urograms / scans – coordinate with CT scans done for colon cancer follow-up, should always include a urogram phase
- Cystoscopy should only be performed if done if retrograde pyelography is done as well
Lastly, he touched on the potential role of Lynch Syndrome (and microsatellite instability) on the role of immunotherapy for UTUC. Due to the nature of their genetic defect, these patients have an even higher rate of mutation rates in the tumor genome than normal UTUC tumors. Hence, they may be acutely sensitive to immune checkpoint blockade. However, further work needs to be done in this space.
Presented by: Alexandre Zlotta, MD, Ph.D., FRCSC, Univerity Urology Associates, Toronto, Canada
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @TjuUrology) at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @TjuUrology) at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.


