
This first slide highlights the fact that the normal pathway (up to) is from a primordial germ cell to gonocyte and eventually to sperm. However, the pathway PGC to testis cancer is now understood to (in many cases) include a hit to the developmental pathway at the 4th week of gestation. Eventually, later in life, this results in the formation of a germ cell neoplasia in situ (GCNIS), which differentiates into seminoma or nonseminomatous germ cell tumor (NSGCT).

However, testis tumors can arise from multiple time points. Type 1 GCC arise from early PGC and present as tumors in infancy. The vast majority present as Type 2 GCC, which present in men in their 20-30’s. On the other extreme, Type 3 GCC present as spermatocytic seminoma in older men.
He then focused on the concept of testicular dysgenesis syndrome (TDS). This is highlighted below:
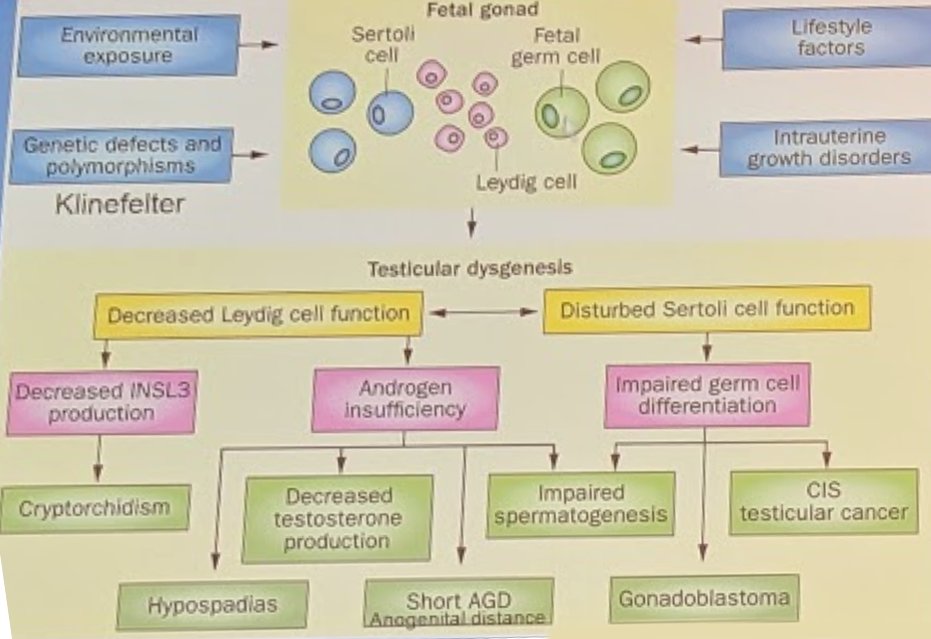
Multiple contributing factors (environmental exposures, genetic conditions, maternal lifestyle factors, and intrauterine growth disorders) have an impact on the fetal gonad. These can lead to testicular dysgenesis, which has an array of downstream clinical manifestations – not just testicular cancer. This includes cryptorchidism, impaired spermatogenesis, CIS / testis cancer, but also hypospadias, gonadoblastoma (in female patients), and short AGD.
Yet, there is a latency period between the hit in the 4th week of gestation to the development of testis cancer (Type II GCC). This is presumed to be due to initiation of puberty-related hormonal changes potentially activating these GCNIS into formal tumors later in life.
The slide below highlights nicely the association between the clinical features of TDS and development of testis cancer, as is very much on a spectrum:
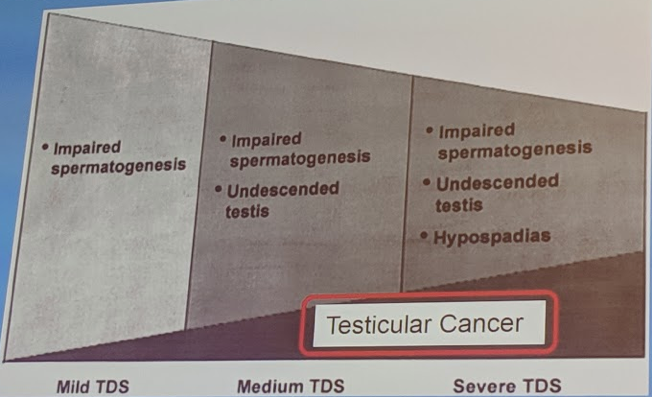
In mild forms of TDS, usually associated with just impaired spermatogenesis, there are very low rates of testis cancer – which is why not all infertile men are at testis cancer risk. Yet, as additional features, such as UDT and hypospadias, are clinically present, the risk of testis cancer significantly increases.
*Ultimately, TDS does NOT equal testis cancer. Men without TDS develop testis cancer. BUT, severe TDS is strongly related to testis cancer development.
He then spent the rest of the talk focusing on other factors in the development of testis cancer, which I will summarize below:
- Environmental/genetic factors – “Genvironmental” factors
- Single gene mutations are very rare in TCa development – numerous GWAS studies have not demonstrated driver mutations, such as in other malignancies. We are unlikely to find single gene actionable mutations in TCa
- Based on the distribution of TCa worldwide, there is a clear environmental component that plays into TCa development – particularly in first-world countries

-The nature of these environmental factors is not entirely certain
- Pesticides, polychlorinated biphenols (PCBs), polyaromatic hydrocarbons, phytoestrogens, and other similar agents have been implicated
- However, much more work is needed to identify which agents impact GCT development, when it occurs and how to prevent it
2) Alternative mechanisms of GNCIS formation
- As men without TDS develop TCa, there must be other mechanisms of development – also as, Type I GCT develop in infancy before puberty and manifestation of TDS, more evidence that other factors play a role
- Work by Looijenga et al. had increased our understanding of epigenetic effects on the normal gonocyte itself that may bypass that 4th week of gestation hit pathway
Presented by: Peter Albers, MD, Professor of Urology, Department of Urology, Düsseldorf University, Germany


