1. Resolution of previous features suspicious on MRI
2. Reduction in volume and/or conspicuity of feature suspicious for prostate cancer
3. Stable MRI appearance: no new focal/diffuse lesions
4. A significant increase in size and/or conspicuity of features suspicious for prostate cancer
5. Definite radiologic stage progression
The aim of this study was to compare the PRECISE score with clinical progression in men who are managed using an MRI-led active surveillance protocol.
For this study, men on active surveillance for low or intermediate risk prostate cancer who had had two or more MRI scans between April 2006 and September 2017 were included (n=150). A total of 535 scans from these men were re-reported by a dedicated radiologist to give a PI-RADS v2 score for each scan, measurement of all lesions, and a PRECISE score for the likelihood of radiological progression. Clinical progression was defined by histological progression to ≥ Gleason Grade Group 3 and/or initiation of active treatment. Subsequently, the tumor growth rate between serial scans was calculated.
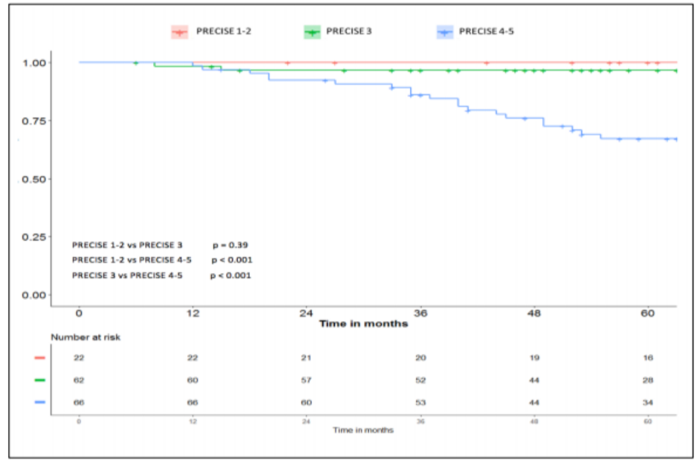
Dr. Giganti and colleagues found that freedom from clinical progression at 12, 24 and 60 months for PRECISE 1-2 was 100% at all time points. For PRECISE 3, it was 98.4% at 12 months, 96.7% at 24 months, and 96.7% at 60 months. For PRECISE 4-5, it was 98.5% at 12 months, 92.4% at 24 months, and 67.1% at 60 months. There was a significant difference between PRECISE 1-2 vs 4-5 and PRECISE 3 vs 4-5 (p<0.001). This Kaplan-Meier curve shows the rate of clinical progression stratified by PRECISE score:
Fifty-six men (37%) had a visible lesion on all scans, and their tumor growth rate by planimetry was higher with higher PRECISE scores (all p<0.05). The authors note that limitations of their study include the fact that serial biopsies were not routinely performed and that the biopsy approach varied (standard vs targeted), thus potentially introducing heterogeneity into the results. Perhaps with increased sample size, there may be utility in stratifying PRECISE score 4 and 5 separately.
Dr. Giganti’s conclusions from this study are as follows:
- Radiological stability (PRECISE 1-3) in men on AS is associated with a high rate of freedom from clinical progression.
- If men had clinical progression, then this was almost always detectable on MRI.
- Men with a stable MRI had a very low likelihood of clinical progression and many could avoid routine re-biopsy.
Presented by: Francesco Giganti, University College London, Division of Surgical and Interventional Sciences, London, United Kingdom
Written by: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University - Medical College of Georgia, Twitter: @zklaassen_md at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.
References:
1. Moore CM, Giganti F, Albertsen P, et al. Reporting Magnetic Resonance Imaging in Men on Active Surveillance for Prostate Cancer: The PRECISE Recommendations—A Report of a European School of Oncology Task Force. Eur Urol 2017 Apr;71(4):648-655.


