Many factors are needed to run a clinic and a service that can provide all the needs of patients treated with immune checkpoint inhibitors. These include knowledgeable nurses, monitoring abilities, 24-hour emergency staff with a clear emergency plan, and a multidisciplinary team.
Before prescribing immune checkpoint inhibitors, physicians must educate the patients on this specific, novel and unique treatment, including the patient’s family and friends. This should be done before and during treatment, and be provided to the patient in an inviting and accessible manner. The patient should be educated on the prophylaxis, side effects and be given practical information about the upcoming treatment. Aside from the physician, the patient should also meet and discuss with a qualified nurse, who should continue to educate the patient, provide information on prophylaxis and side effects, and also give practical information on what to do in different situations.
Before commencing treatment, pretreatment history must be collected from the patient. This includes information on previous autoimmune, infectious, endocrine, and organ-specific diseases, and also knowledge on the patient’s baseline bowel habits. The patient must be evaluated, and diagnostic tests need to be done. These include the common blood tests and more, including CBC, full biochemistry panel, thyroid function tests, urinalysis, specific virology tests (hepatitis B, C and HIV, Epstein Bar and CMV), and also a test for tuberculosis. Patients must be given an extensive wallet card consisting of all relevant information, and the patient should carry this at all times.
Next, the topic of infusion reaction was discussed. This usually occurs with the first dose of treatment and manifests as fever, rash, pruritus, hypotension, tachycardia, dyspnea, and chest discomfort. It occurs in less than 10% of approved immune checkpoint inhibitors, and with avelumab, the frequency is approximately 25%. When this does occur, it is important to reduce the infusion rate, administer saline infusion, anti-allergic therapy and steroids, and before giving the next treatment of immune checkpoint inhibitors, the patient needs to be premedicated with diphenhydramine and paracetamol.
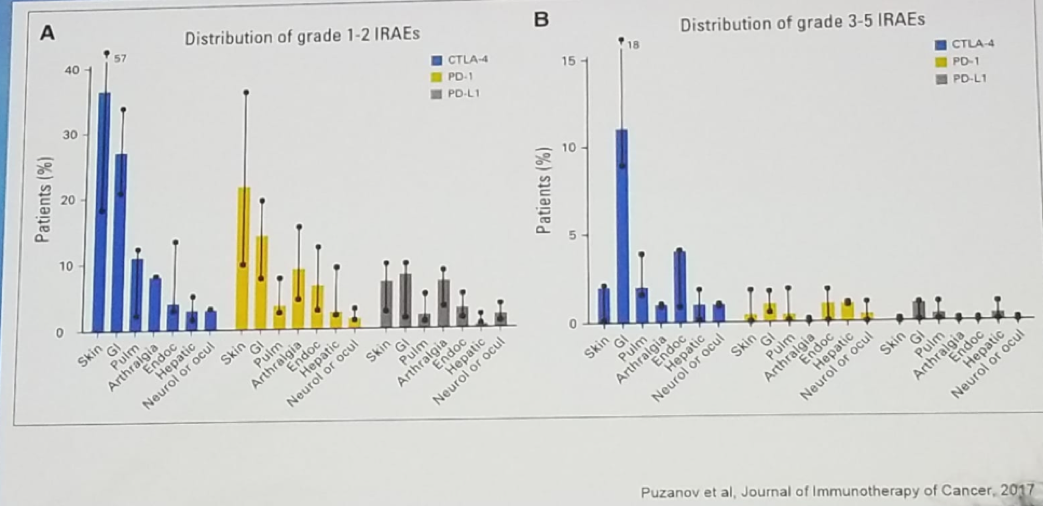
When the patient is given therapy, concise and elaborate documentation is mandatory, and every step of the treatment should be clear to the staff treating the patient and to the patient. If any adverse effects develop, this must be recorded, and proper treatment administered. The managing clinic should always have emergency medications available if needed, such as steroids. The treating physician should have extensive knowledge on the plethora of potential adverse effects (Figure 1) that can be caused by immune checkpoint inhibitors, and he/she should also know how to treat them effectively.
Figure 1 – The vast possible adverse effects of immune checkpoint inhibitors:
The complication of superinfection was discussed next. This occurs in 3% of patients treated with monotherapy (PD-1/PD-l1), and in 10% of patients treated with combination therapy (PD-1/PD-L1 and CTLA4). The possible symptoms include cough, dyspnea, wheezing, chest pain, fatigue, and fever. Sometimes there are no symptoms and just signs of pneumonitis are witnessed. The differential diagnosis included bacterial or viral infection, reactivation of sarcoidosis, cardiac insufficiency, chronic obstructive pulmonary disease, pulmonary hypertension, pulmonary embolus, and lymphangitis carcinomatosa. The possible organisms that can cause superinfection include Pneumocystis jiroveci, legionella, chlamydia, mycoplasma pneumonia, influenza virus, metapneumovirus, and respiratory syncytial virus. In these cases, it is required to perform several diagnostic tests, including a CT scan, pulse oximetry, and for grade>=2 complications –nasal, sputum, and blood cultures should be obtained together with bronchoscopy with lavage, and lung biopsy is indicated if an unexplained/suspicious lesion exists.
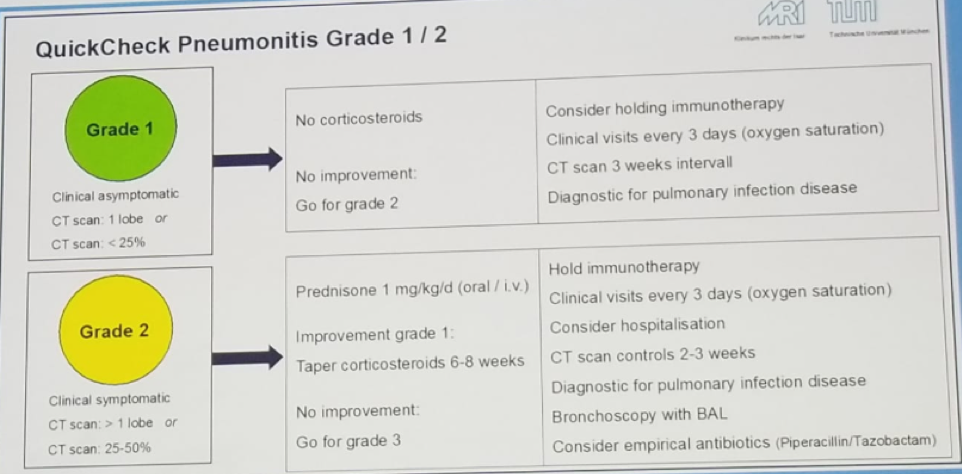
Next, the topic of pneumonitis, a common complication with immune checkpoint inhibitor treatment, was discussed. Table 1 summarizes the treatment of this complication according to its grading.
Table 1 – Treatment of pneumonitis according to its grading:

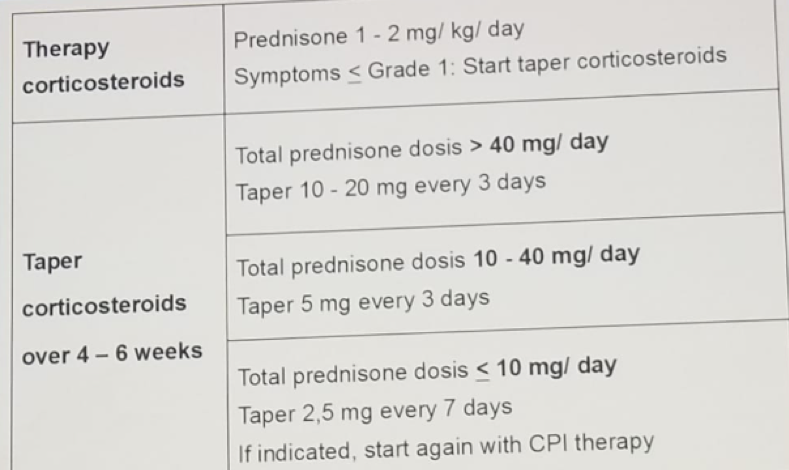
If deciding that the patient requires steroids, the physician should be aware of the adverse effects caused by this medication, and what drugs need to be administered to limit some of the side effects. These include prevention of infections brought by steroids, proton pump inhibitor for gastritis, calcium and vitamin D3 for osteoporosis, oral care to prevent oral candidiasis, blood glucose monitoring for diabetes, blood lipids for hyperlipidemia, cardiovascular examination for hypertension, and ophthalmological examination for cataract and glaucoma. It is also most important that treating physicians know how to correctly taper steroids. A suggested schedule of how to taper steroids is shown in table 2.
Table 2 – How to taper steroids:
The last topic discussed in this session was one of the more common complications of immune checkpoint inhibitors, which is hypothyroidism. It usually manifests with symptoms of headache, fatigue, adynamia, nervousness, blurred vision, dizziness, hypotension, metabolic panel disorders, polyuria, and polydipsia. Sometimes it can manifest as a life-threatening disorder with hypophysitis, and adrenal insufficiency. It is critical to obtain blood tests, including basic metabolic panel, ACTH, Cortisol level, TSH, T3, T4, LH and FSH, testosterone and estrogen, and perform a brain MRI if there is associated blurred vision. An algorithm explaining how to diagnose and treat the complications of hypothyroidism and hyperthyroidism is shown in figure 2.
Figure 2- How to diagnose and treat hypothyroidism/hyperthyroidism:

Presented by: Margitta Retz, MD, Department of Urology, Klinikum rechts der Isar der Technischen Universität München, Munich, Germany
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019


