(UroToday.com) The 2024 European Association of Urology (EAU) annual meeting featured a plenary session on personalized approaches in high-risk and metastatic prostate cancer, and a state of the art lecture by nuclear medicine physician Dr. Irene Burger discussing strengths and pitfalls of staging high-risk prostate cancer with PSMA PET.
Dr. Burger started by highlighting that most/all of the best evidence supporting staging high-risk prostate cancer with PSMA PET comes from the proPSMA trial.1 This was a prospective, randomized, multi-center clinical trial of men with at least one high-risk factor including PSA >= 20 ng/mL, ISUP grade group 3-5, or clinical stage T3 or greater. Following enrollment, patients were randomly assigned in a 1:1 ratio to either conventional imaging performed using bone scan and CT or PSMA PET/CT. Among 302 patients randomized, in the primary outcome assessment, PSMA PET-CT had a 27% absolute greater AUC for accuracy compared to conventional imaging (95% CI 23-31): 92% (95% CI 88-95%) vs. 65% (60-69%). These results are further supported by assessing improvement in the staging of pelvic nodal and distant metastases:
However, Dr. Burger notes that PSMA PET staging of lymph nodes is still not perfect. Data from retrospective studies suggests that sensitivity rates at the patient level are ~65% and at the lymph node field level are ~74%, with the majority of missed lymph nodes < 5 mm. In a recent meta-analysis of 2,431 patients, PSMA-PET significantly outperformed conventional imaging, suggesting that PSMA-PET should be used as a first-line approach for the initial staging of prostate cancer:2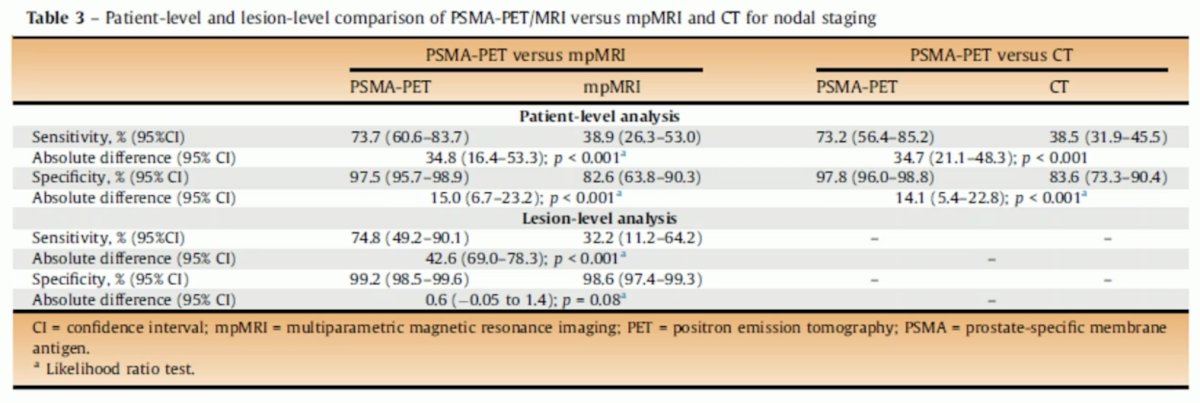
Additionally, PSMA PET is as good as the MSKCC nomogram and the Partin tables for predicting positive lymph nodes:3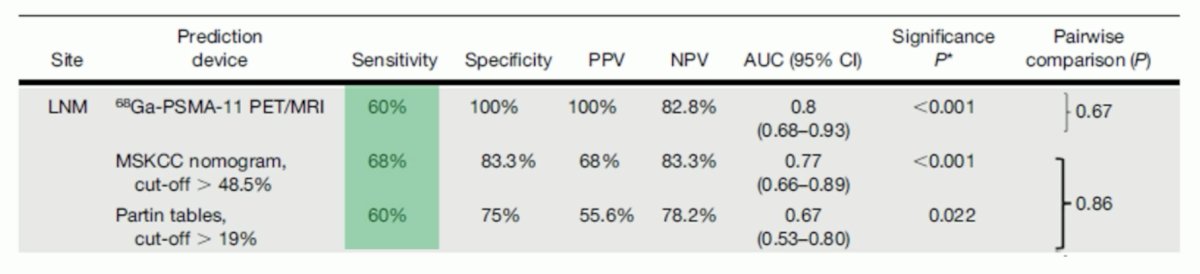
Moreover, nomograms for lymph node detection are now incorporating PSMA PET staging. For example, Muehlematter et al. used a combined model that included PSA, biopsy Gleason grade group, 68Ga-PSMA-11 positive volume of the primary tumor, and the assessment of the 68Ga-PSMA-11 report N-status.4 This model yielded an AUC of 0.923 (95% CI 0.863-0.984) in the external validation, and using a cutoff of ≥ 17%, 44 (50%) extended pelvic lymph node dissections would be spared and lymph node invasion missed in one patient (4.8%). This compares very favorably to the other available nomograms: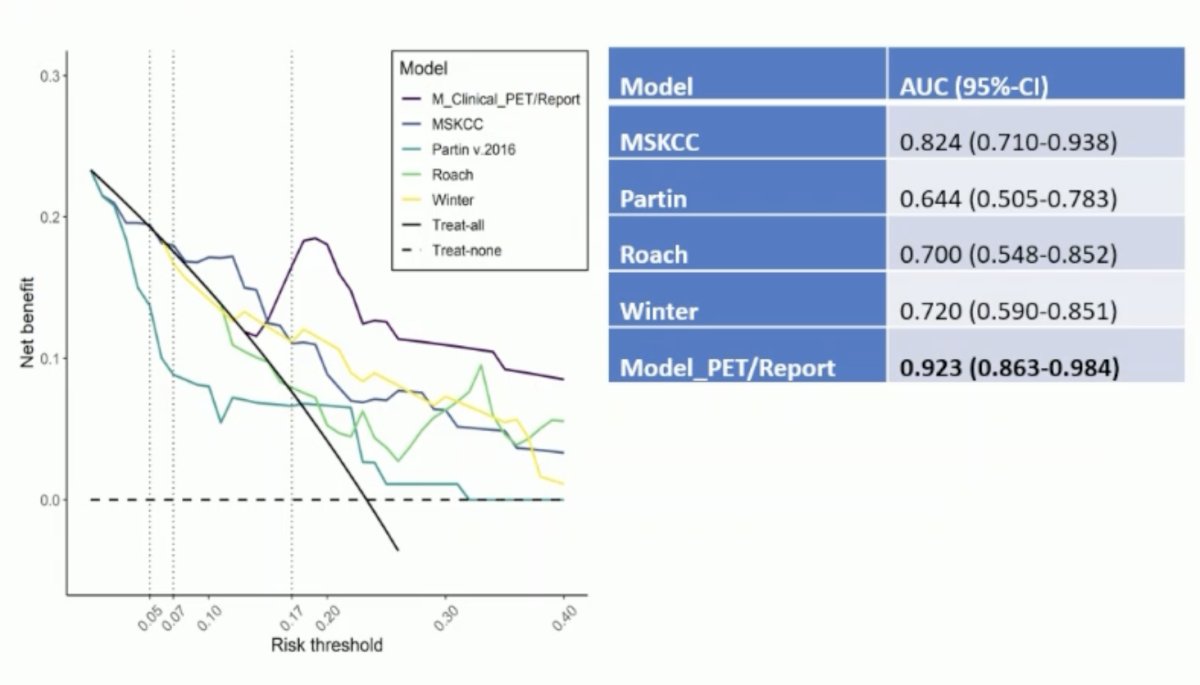
The overall impact of PSMA PET/CT is important. Data from proPSMA suggests that imaging findings led to changes in management (treatment intent, modality, or delivery) in 28% of men in the PSMA PET/CT arm versus 15% of men in the conventional imaging arm.1 Following first-line PSMA PET/CT, 20 (14%) of 148 patients were directed from curative to palliative-intent treatment, 11 (7%) had a change in radiotherapy technique, and 11 (7%) in surgical technique. Notably, conventional imaging was associated with a higher radiation dose (19.2 mSv compared to 8.4 mSv; absolute difference 10.9 mSv, 95% CI for difference: 9.8 – 12.0 mSv). PSMA PET-CT was not associated with any adverse events and reporter agreement was high for both nodal (kappa=0.87, 95% CI: 0.81 – 0.94) and distant metastatic disease (kappa=0.88, 95% CI: 0.84 – 0.92).
Considering the evaluation of local extension, several studies suggest that PSMA PET/CT has slightly improved sensitivity for assessing extracapsular extension and seminal vesicle invasion compared to MRI, with comparable specificity: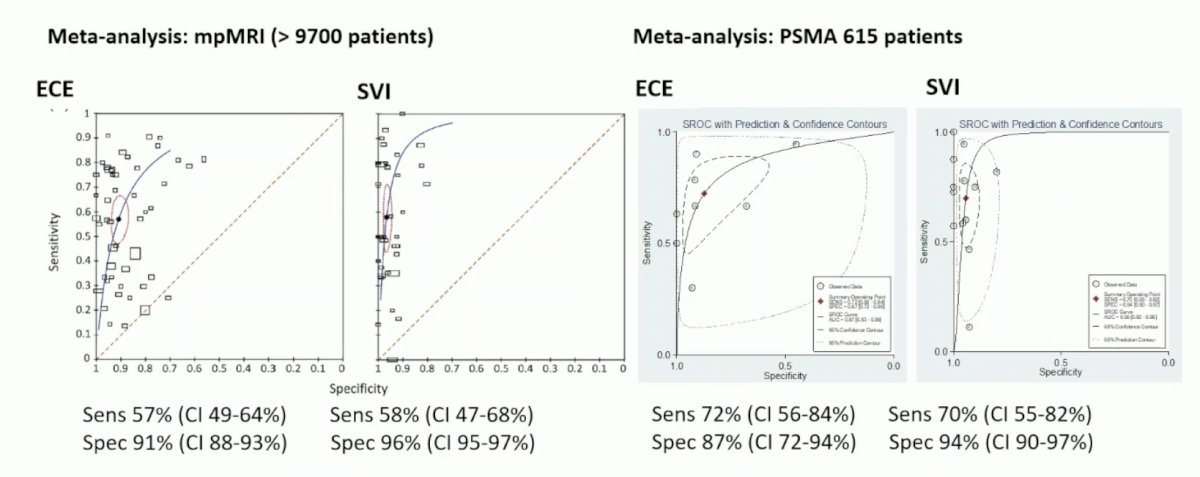
The final portion of Dr. Burger’s talk focused on PSMA pitfalls, starting with the pitfall of false positives. This may be within the prostate gland (specifically in the central zone), within the lymph nodes (uptake in ganglia/neurinoma, inflammation, etc), or within the bones (hemangiomas, Paget’s disease, fibrous dysplasia, “unspecific bone uptake”, etc):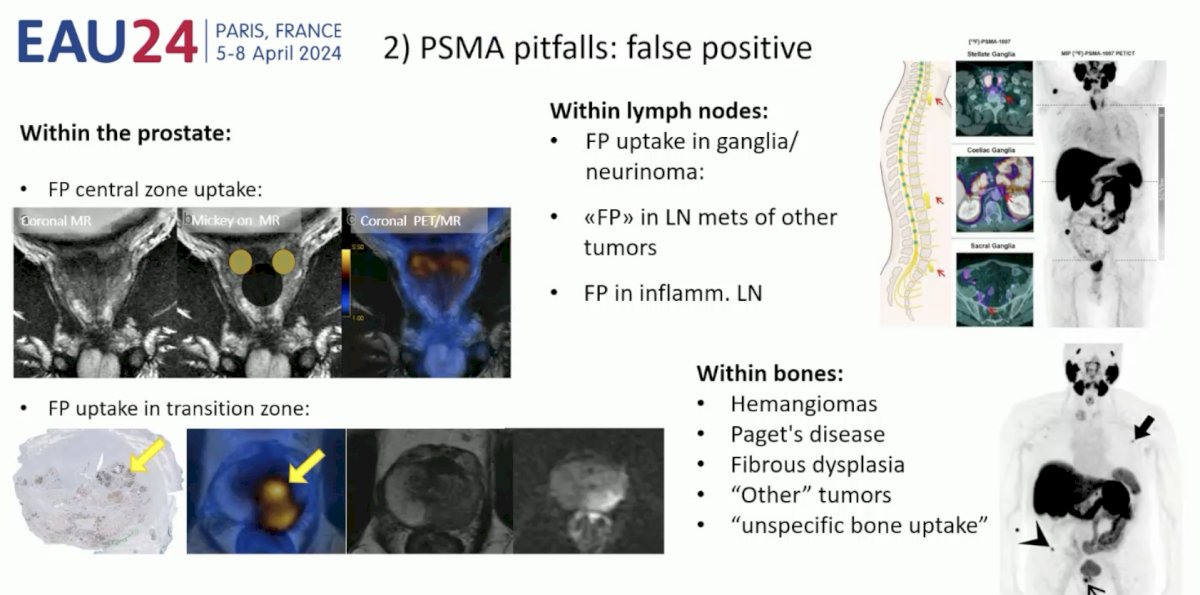
To conclude, Dr. Burger notes that there may also be PSMA false-negative findings, particularly in the intra-prostatic assessment of Grade Group: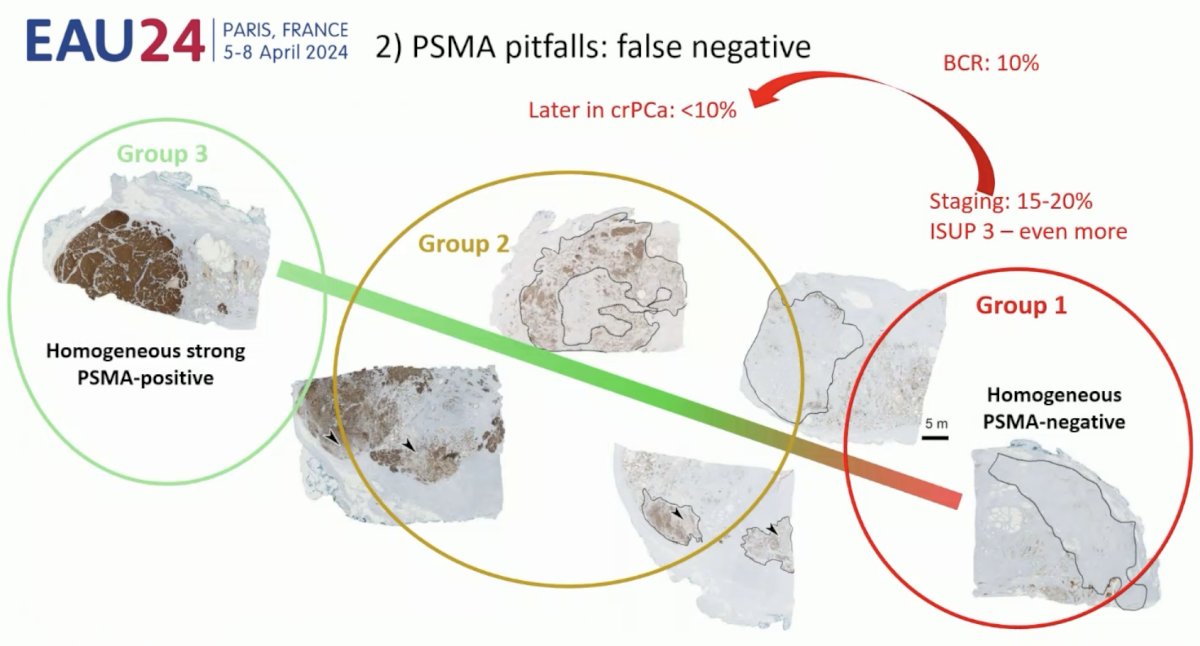
Presented by: Irene Burger, MD, Kantonsspital Baden, Baden, Switzerland
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, WellStar MCG Health, @zklaassen_md on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th - April 8th, 2024
References:
- Hofman MS, Lawrentschuk N, Francis, RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): A prospective, randomized, multicentre study. Lancet 2020 Apr 11;395(10231):1208-1216.
- Chow KM, So WZ, Lee HJ, et al. Head-to-head comparison of the diagnostic accuracy of prostate-specific membrane antigen positron emission tomography and conventional imaging modalities for initial staging of intermediate- to high-risk prostate cancer: A systematic review and meta-analysis. Eur Urol. 2023 Jul;84(1):36-48.
- Maurer T, Gschwend JE, Rauscher I, et al. Diagnostic efficacy of (68)Gallium-PSMA positron emission tomography compared to conventional imaging for lymph node staging of 130 consecutive patients with intermediate to high-risk prostate cancer. J Urol. 2016 May;195(5):;1436-1443.
- Muehlematter UJ, Schweiger L, Ferraro DA, et al. Development and external validation of a multivariable [68Ga]Ga-PSMA-11 PET-based prediction model for lymph node involvement in men with intermediate or high-risk prostate cancer. Eur J Nucl Med Mol Imaging. 2023 Aug;50(10):3137-3146.


