Ultimately, the question is whether locoregional control halts disease progression and metastases. Previous surgical data suggests that in patients with cN0 disease the internal iliac lymph nodes may be positive in 58% of patients, and internal iliac lymph nodes alone may be positive in 19% of patients. Thus, a lymph node dissection along the internal iliac (hypogastric) vessels is essential for representative staging. There are several important considerations for using lymph node dissections for correctly staging patients, including (i) extended pelvic lymphadenectomy being the most accurate staging procedure, (ii) accurate staging may inform and improve future decision making, and (iii) >30% of cN1 patients are in fact pathologically negative.
In a study from Dr. Touijer’s groups assessing long-term outcomes of 369 patients with lymph node metastasis treated with radical prostatectomy without adjuvant ADT, 64 patients with lymph node metastasis died, including 37 from the disease.1 Overall, 70 patients developed metastasis, and 201 experienced biochemical recurrence. The predicted 10-year overall survival was 60% (95% CI 49-69) and cancer-specific survival was 72% (95% CI, 61-80). The 10-year probability of freedom from distant metastasis and freedom from biochemical recurrence was 65% (95% CI, 56-73) and 28% (95% CI, 21-36), respectively. From this study, Dr. Touijer concluded that a considerable subset of men with lymph node metastasis will remain disease-free 10 years after radical prostatectomy and extended lymph node dissection alone.
Furthermore, the EAU guidelines suggest that for patients with locally-advanced disease, clinicians may offer a radical prostatectomy in highly selected patients with cT3b-T4N0 or any T N1 as part of multimodal therapy.2 For these patients, they should also undergo an extended pelvic lymph node dissection given their high-risk prostate cancer.
One challenge, according to Dr. Touijer, is how we define cN1 disease. Pooled data suggest that CT is only 42% sensitive and 82% specific, whereas MRI is only 39% sensitive and 82% specific. Cross-sectional imaging relies on size and morphology considerations, including >=1 cm in length, roundness, and loss of a fatty hilum. Data from Dr. Touijer’s group showed that in an assessment of pathological features of lymph node metastasis for predicting biochemical recurrence after radical prostatectomy, the median metastatic lymph node diameter was only 9 mm (IQR 5-16).3 Recent data from the proPSMA study assessed prostate-specific membrane antigen (PSMA) PET in patients with high-risk prostate cancer before either radical prostatectomy or radiotherapy.4 Among 302 men eligible, 152 (50%) were randomly assigned to conventional imaging and 150 (50%) to PSMA PET-CT. Of 295 (98%) men with follow-up, 87 (30%) had pelvic nodal or distant metastatic disease, and PSMA PET-CT had a 27% (95% CI 23-31) greater accuracy than that of conventional imaging (92% [95% CI 88-95] versus 65% [95% CI 60-69]; p<0.0001) for detecting nodal disease. Additionally, there was a lower sensitivity (38% [95% CI 24-52] versus 85% [95% CI 74-96]) and specificity (91% [95% CI 85-97] versus 98% [95% CI 95-100]) for conventional imaging compared with PSMA PET-CT.
Taken together, there is a disconnect between the size of positive nodes (median ~4 mm) and the ability of preoperative imaging to detect these nodes: PSMA avid median diameter 7mm; mpMRI median diameter 11.7 mm. Additionally, up to 35% of lymph nodes land outside the site of an extended template lymph node dissection. 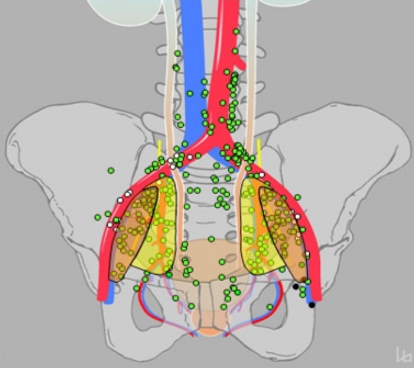
Several challenges that should be part of future directions according to Dr. Touijer include (i) micrometastatic nodes that undetectable by modern imaging, and (ii) micrometastatic nodes on PSMA PET that are outside the extended pelvic lymph node dissection template. The age-old question of whether there is an oncological benefit to treat the lymph nodes will be attempted to be answered by two clinical trials: 1) Role of Lymph Node Dissection in Men with Prostate Cancer Treated with Radical Prostatectomy (PREDICT) and 2) Trial Modifications to Radical Prostatectomy: PLND versus no PLND.
To conclude, Dr. Touijer noted that:
- Extended pelvic lymph node dissection is the most accurate staging procedure
- Staging accuracy helps guide future multidisciplinary decision-making
- PSMA based image-guided surgery/radiation is promising
Presented by: Karim A. Touijer, MD, MPH, Memorial Sloan Kettering Cancer Center, New York, NY
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
References:
- Touijer KA, Mazzola CR, Sjoberg DD, et al. Long-term outcomes of patients with lymph node metastasis treated with radical prostatectomy without adjuvant androgen-deprivation therapy. Eur Urol 2014 Jan;65(1):20-25.
- Mottet N, Bellmunt J, Bolla M, et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening Diagnosis, and Local Treatment with Curative Intent. Eur Urol 2017;71(4):618-629.
- Carlsson SV, Tafe LJ, Chade DC, et al. Pathological features of lymph node metastasis for predicting biochemical recurrence after radical prostatectomy for prostate cancer. J Urol 2013;189:1314-1319.
- Hofman MS, Lawrentschuk N, Francis, RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): A prospective, randomized, multicentre study. Lancet 2020 Apr 11;395(10231):1208-1216.


