The principle of triage in cancer diagnosis is well established across medicine. Investigative strategies must balance false negatives, overdiagnosis, and the morbidity of investigation. Rates of false-negative of mammography (6-46%) and cystoscopy (10-40%) are not insignificant. Dr. Ahmed stressed the role of prostate Magnetic resonance imaging (MRI) as a triage test to avoid initial upfront prostate biopsy.
He emphasized that ongoing follow-up of these patients would occur to avoid risks of false-negative tests.
He began by recapping the PROMIS study, as it gives important information on the false negative rates of prostate MRI. In this study, men underwent MRI, TRUS biopsy, and a transperineal mapping biopsy.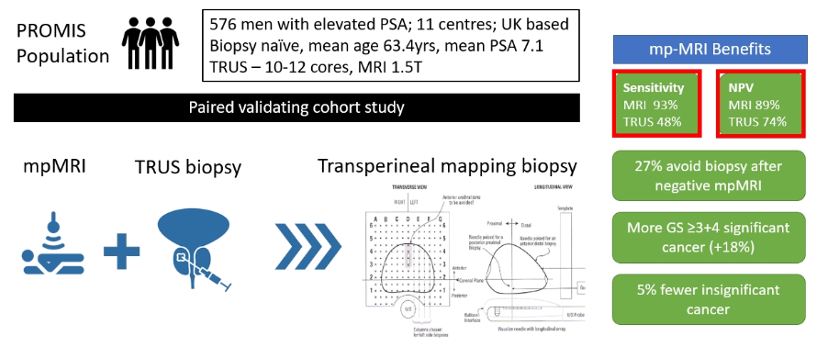
This study demonstrated that, while MRI missed some GS 3+4 tumors, a MRI guided approach reduced clinically insignificant cancers and increased clinically significant cancer compared to a TRUS-biopsy based strategy.
In a systematic review aimed at assessing the negative predictive value of mpMRI, Dr. Ahmed highlighted data from a group led by Alastair Lamb which demonstrated a pooled NPV of 91%.
Going back to the PROMIS study, patients with MRI missed cancers ad predominately less aggressive disease, with no cases of missed 3+5, 4+3, 4+5, or 5+4 disease.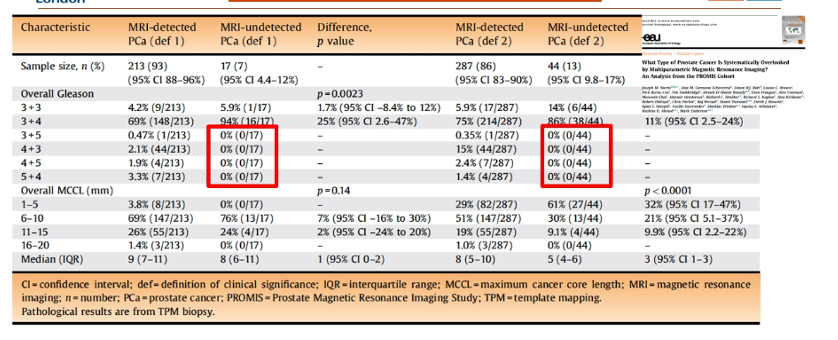
Further, a comparison of systematic transrectal ultrasound (TRUS) guided biopsy. results with PiRADS based Likert scores demonstrate a low rate of clinically significant disease (1: 0%; 2: 2%) in the PROMIS cohort suggesting that the omission of systematic biopsy for men with a negative MRI is unlikely to miss clinically relevant disease that would have been detected on systematic TRUS biopsy. A systematic review demonstrated comparable results with 8% clinically significant disease in those with a normal MRI.
Dr. Ahmed further highlighted data that the combination of MRI results and PSA density may provide further beneficial risk stratification. Namely, in men with a normal MRI and a low PSA density, the negative predictive value is in excess of 90% and may be as high as 97% in patients with a PSAD <0.10. Further, in patients with PiRADS 3 lesions, use of a PSAD cut off of 0.15 may allow the avoidance of more than 40% of biopsies without meaningfully increasing the miss of clinically significant disease.
In patients with negative MRI without initial biopsy, rates of clinically significant cancer over a 5 year follow-up is low (less than 5%) suggesting that there is not a meaningfully high rate of miss for clinically significant disease through the omission of upfront biopsy.
Presented by: Hashim U. Ahmed, MD, Ph.D., BM, Bch, Professor, and Chair of Urology; Consultant Urological Surgeon, Imperial College London, Great Britain
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter at the 35th Annual EAU Congress, 2020 Virtual Program #EAU20, July 17-19, 2020.


