(UroToday.com) As part of a plenary presentation at the virtual 2020 European Association of Urology (EAU) Annual Meeting assessing “Modern prostate cancer imaging in daily practice,” Bertrand Tombal, MD, PhD, followed Annika Herlemann, MD’s presentation by suggesting we start with early imaging for patients with biochemical recurrence following initial local therapy.
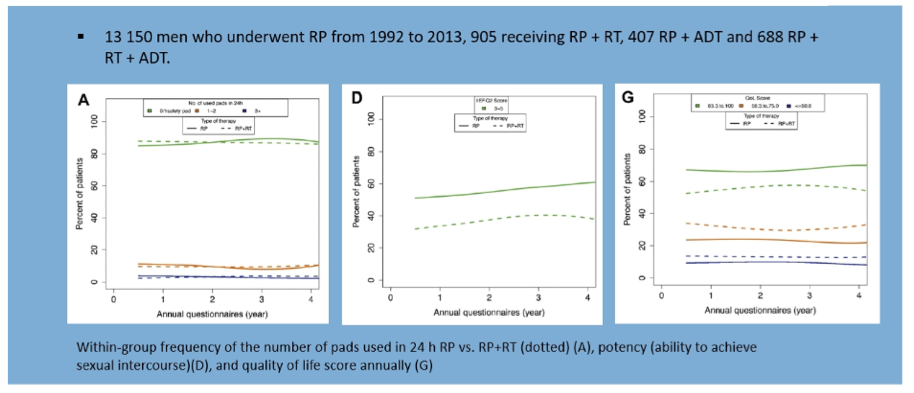
His first argument was that “blind treatment” is associated with only marginal oncological benefit while there is significant toxicity. In addition to unnecessary treatment with such an approach, an additional 30-40% of patients will progress, despite salvage therapy initiated early. Further, the toxicity of salvage radiotherapy is not insignificant with effects of urinary continence, erectile function, and quality of life, as highlighted below:
Further, early initiation of systemic therapy has minimal benefit in terms of either overall or cancer-specific survival as highlighted in observational data in the Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) registry: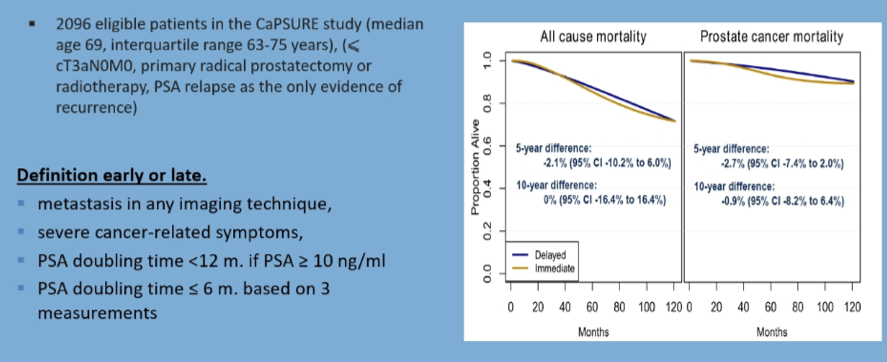
However, randomized data has shown that the early initiation of ADT is associated with improved overall survival, though this comes at the expense of significant toxicity including quality of life.
Beyond the limitations of such “blind treatment”, Dr. Tombal highlighted that new imaging approaches including prostate-specific membrane antigen (PSMA) PET/CT and whole-body magnetic resonance imaging (MRI) consistently demonstrate sites of clinically actionable metastatic disease, including at sites that would not be traditionally considered landing zones.
Highlighting first data on whole-body MRI, Dr. Tombal highlighted data showing much improved diagnostic accuracy compared to bone scan and CT in patients with high-risk disease. Based on the increased ability to detect metastatic disease, this approach allows for better staging.
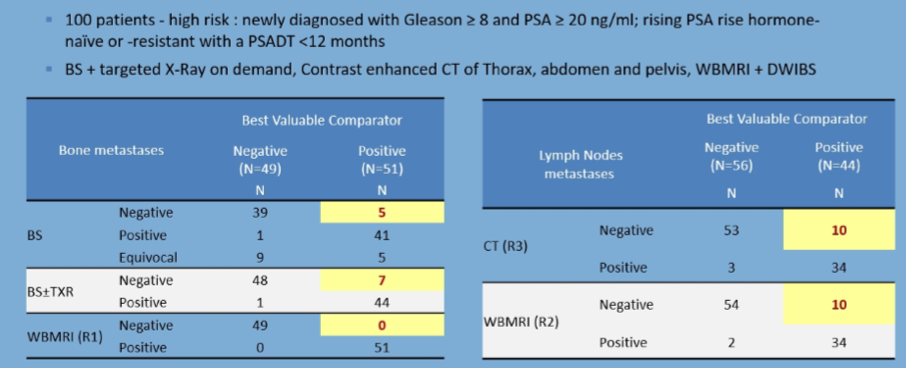
In addition to diagnosing more metastatic disease, use of these newer imaging approaches has shown that nodal disease often occurs in regions beyond standard surgical or RT templates.
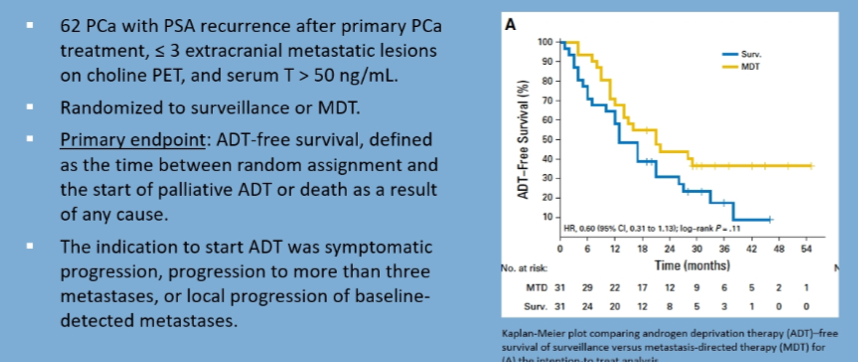
Dr. Tombal then highlighted data showing that metastasis directed therapy can impact treatment outcomes, with a focus on data from Dr. Ost showing improved ADT-free survival.
The Oriole Phase 2 trial has similarly showed a benefit in progression-free survival with the use of SABR as compared to observation.
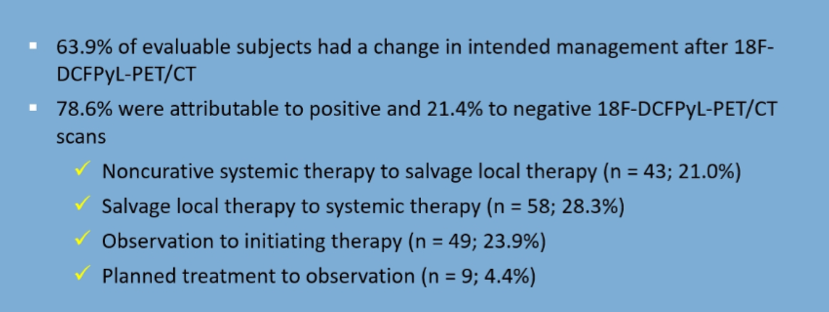
The use of advanced imaging, including PSMA PET/CT, also shows evidence of benefit with increasing the ability to target lesions, including outside expected regions. In the phase III CONDOR study, PET/CT improved the correct localization of recurrent lesions, with changes in intended management in the majority of patients.
Presented by: Bertrand F. Tombal, MD, PhD, Professor and Chairman of the Division of Urology and Associate Professor of Physiology at the Université catholique de Louvain (UCL), Brussels, Belgium
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Nashville, TN, USA, Twitter: @WallisCJD, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
Related Content:
Read — ASCO 2020: Results from a Phase III, Prospective, Multicenter Study (CONDOR): Impact of PSMA-Targeted Imaging with 18F-DCFPyL-PET/CT on Clinical Management of Patients with Biochemically Recurrent Prostate Cancer


