Half of the patients diagnosed with muscle-invasive bladder cancer are older than 75 and have associated comorbidities with polypharmacy and potential cognitive difficulties. They also have frequent undernutrition and sarcopenia. These all pose major risk factors for postoperative complications.
There are many preoperative tools that are routinely utilized to assess surgical fitness, with the most common ones being the performance status and the American Society of Anesthesiologists (ASA) score.
Frailty is defined as an increased vulnerability to adverse health outcomes. It is affected by the accumulation of age and disease-related deficits, and it is an independent risk factor for postoperative morbidity, mortality, and length of hospital stay.
Frailty has a direct correlation to the risk of mortality in almost all surgeries, including radical cystectomy (Figure 2).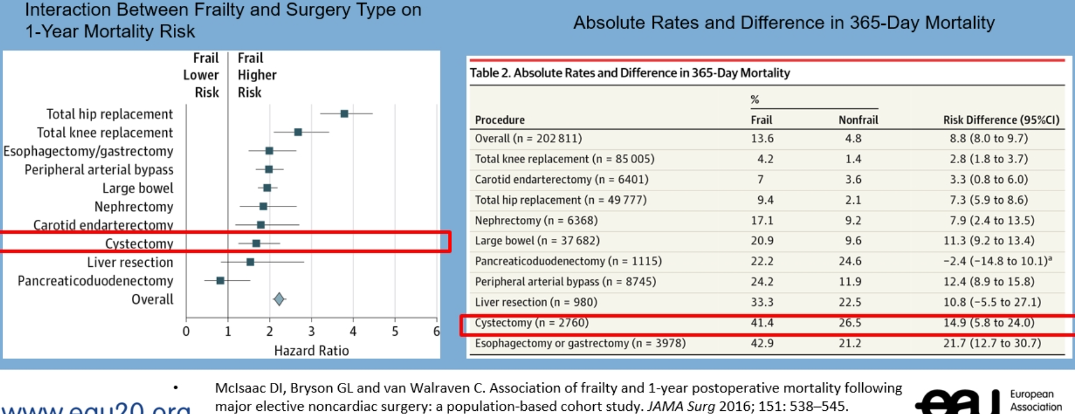
Figure 2. Frailty and mortality in various surgeries
Surgeons should optimize patients preoperatively. This is especially true for large procedures such as radical cystectomy. By doing this, surgeons can avoid postoperative complications an optimize surgical outcomes (Figure 3).
Figure 3. Frailty and radical cystectomy
It is critical that patients who are at risk are preoperatively identified and that the best tools are used for optimization. There are several recommended frailty assessment tools, as can be seen in Table 1.
Table 1. Recommended frailty assessment tools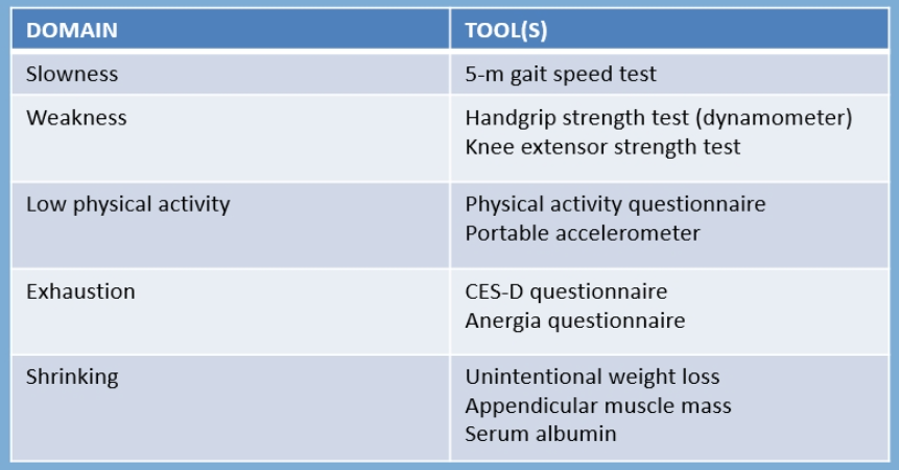
Dr. Géraldine Pignot recommends using the FRIED criteria and FRAIL scale in preoperative identification and optimization of patients (Figure 4). The frailty phenotype is affected by different pathophysiological pathways, as seen in Figure 5.
Figure 4. FRIED criteria and FRAIL scale
Figure 5. Different pathophysiologic pathways leading to the frail phenotype
Sarcopenia is defined as a reduction in muscle mass and or muscular function. Approximately 70% of patients facing radical cystectomy have sarcopenia, which has been associated with high-risk of toxicities during neoadjuvant chemotherapy, high-risk of complications postoperatively, and it also negatively impacts survival. It is, therefore, critical for the preoperative assessment to include muscle mass, muscular strength, and muscular function. This can be done using the skeletal muscle index that is assessed on CT scans (Figure 6). Muscular strength can also be assessed using the handgrip strength test, and muscular function can be assessed with a short physical performance battery, which is a simple combination of short physical tests.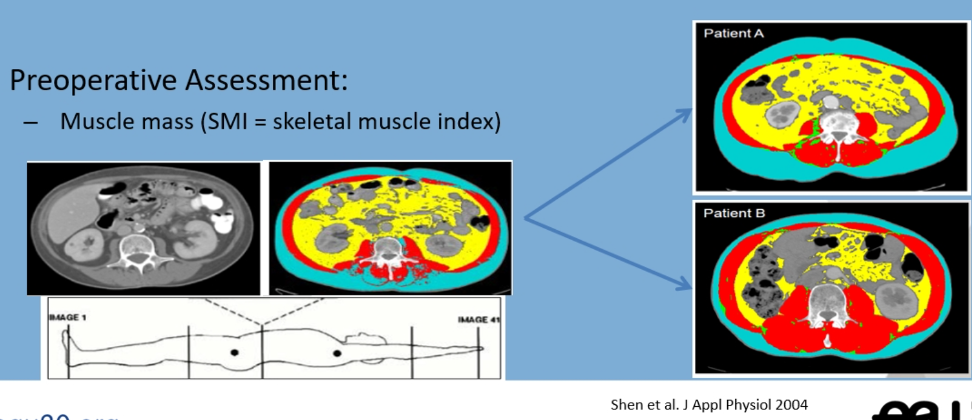
Figure 6. Skeletal muscle index assessment
The definition of undernutrition is an inadequate intake of food to meet the minimal nutritional requirements. It is critical to assess the nutritional status before surgery with the mini nutritional assessment (MNA) test (Figure 7). If undernutrition is diagnosed, preoperative corrective measures are needed, using the ESPEN guidelines (Figure 8).
Figure 7. Undernutrition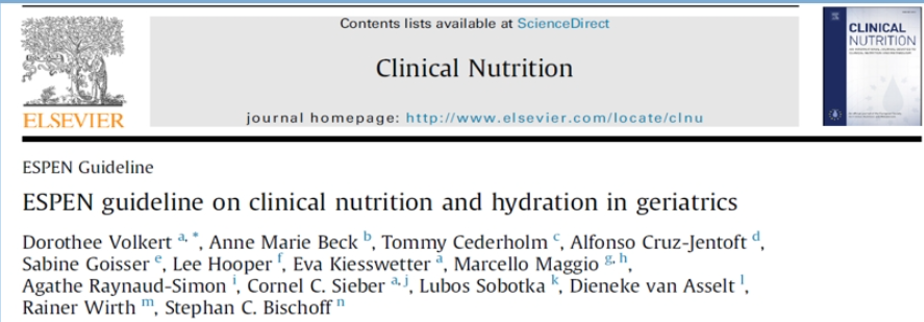
Figure 8. ESPEN guidelines in clinical nutrition
It is also critical to preoperatively identify patients at risk of postoperative delirium, which has been associated with increased morbidity (falls, fractures, sepsis) longer length of hospital stay, and decline in cognitive ability during the first year after surgery. Delirium has many precipitating and predisposing factors, as seen in Figure 9. Preoperative cognitive assessment is critical and should include information about previously known dementia, memory impairment, behavioral disorders, and history of prior postoperative confusion. The assessment should include a mini-COG (three-item recall, and clock drawing), and mini-mental state examination (MMSE). If a cognitive disorder is diagnosed (apart from known dementia), an organic etiology should be sought out, and all measures should be undertaken to avoid postoperative delirium (Figure 10).
Figure 9. Delirium predisposing and precipitating factors
Figure 10. What to do when cognitive disorders are diagnosed?
Dr. Pignot concluded her talk with several important statements. The recognition of frailty is an important consideration in the perioperative period. Neoadjuvant chemotherapy and cystectomy are not contraindicated in frail patients, but caution is needed. Accurate assessment of patients in terms of frailty, multimorbidity, and functional status may allow better modification and shared decision making, leading to improved postoperative outcomes in patients undergoing radical cystectomy.
Presented by: Géraldine Pignot, MD, Urology Surgeon, Institut Paoli-Calmettes, Marseille, France
Written by: Hanan Goldberg, MD, MSc, Urology Department, SUNY Upstate Medical University, Syracuse, New York, Twitter: @GoldbergHanan at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020


