Background / Rationale: Upper tract instillations are considered adjuvant therapy (for high-risk tumors after complete eradication in a kidney sparing approach) or curative (for CIS of the upper tract). At least, that’s the intention. However, there is still a 30-50% recurrence rate requiring frequent surveillance. In terms of progression, it ranges from 5-10% (in the CIS curative setting) to 50% (in the Ta/T1 adjuvant setting); kidney sparing rates are similar (5-10% for CIS and 20-30% for Ta/T1).
The use of adjuvant instillations is not based on the strongest evidence (Level 3, comparator studies and case reports) but randomized control trials would not be ethical due to the high cure rate. Additionally, for CIS of the bladder, cystectomy is not the standard of care – so why should radical nephroureterectomy be standard for UTUC CIS?
Hence, he makes the cases that upper tract instillation saves kidneys and is the standard of care for UTUC CIS.
Techniques
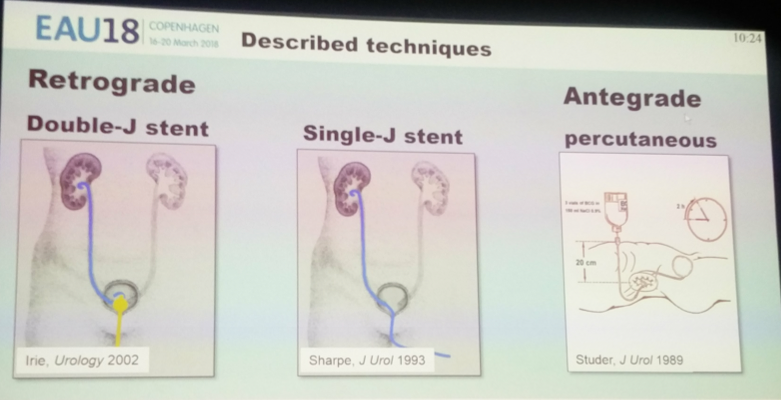
There are three primary options for upper tract instillation:
1. Retrograde
a. Double-J stent placement, instillation in bladder – works through bladder reflux
b. Single-J stent, direct instillation into the upper tract
2. Antegrade
a. Nephrostomy tube, direct instillation into the upper tract
The three main considerations are:
1. Treatment efficacy
2. Safety
3. Patient friendliness, tolerability
1. Retrograde injection via double-J stent – patient in trendelenberg, intravesical BCG for 30-120 minutes
a. Treatment efficacy is poor - 44% of patients were found to not have reflux!
2. Retrograde injection via double-J stent – patient in trendelenberg position, 1-hour continuous infusion. Repeated instrumentation during each visit.
a. Foreign body in ureter and bladder, may prevent adequate contact of instilled agent to mucosa
b. No control of the flow rate, so intrapyelic pressures may be high or low – if too high, may be dangerous, if too low, ineffective
3. Percutaneous antegrade instillation via nephrostomy tube – pre-placed nephrostomy maintained during duration of therapy, continuous flow for 2 hours, control of flow.
a. Flow rate controlled – intrapyelic pressures are controlled
b. Unobstructed flow, no issue with mucosal contact
c. Patient has to be ok with external tube for duration of therapy
d. Minimal Grade 3-4 adverse events
e. No tumor seeding has been found along the tract, even on long term follow-up (Giannanni, EU 2011)
Per Dr. Seiler, the antegrade approach is the preferred approach.
Presented by: R. Seiler, Bern, Switzerland
Written by: Thenappan Chandrasekar, MD Clinical Fellow, University of Toronto, twitter: @tchandra_uromd at the 2018 European Association of Urology Meeting EAU18, 16-20 March, 2018 Copenhagen, Denmark


