In the setting of active surveillance of low-grade prostate cancer, there is some similarity in the various guidelines regarding the recommendation of performing a mpMRI. CCO recommends performing mpMRI when a patient’s clinical findings are discordant with the pathologic findings. The national comprehensive cancer network (NCCN) recommends considering mpMRI if anterior and/or aggressive cancer is expected (when PSA is increased and systematic biopsies are negative). Lastly, the National institution for health and care excellence (NICE) guidelines recommend a mpMRI at enrollment to active surveillance.
In the setting of pre-treatment local staging of prostate cancer, the CCO states that it is reasonable to perform a mpMRI to assess extra-prostatic extension in intermediate and high-risk patients considered for radical therapy (if knowledge of extraprostatic extension will alter management). Centers following this recommendation must have a quality assurance program to measure the diagnostic performance of mpMRI.
The indication for mpMRI use according to the CCO include:
- High PSA with a prior negative systematic biopsy
- Active surveillance – in changing the risk profile
- Staging – intermediate and high risk if it will alter management
- Reassessment after local therapy
- Local recurrence - only if it will alter management
- High PSA with no previous biopsies – not recommended!
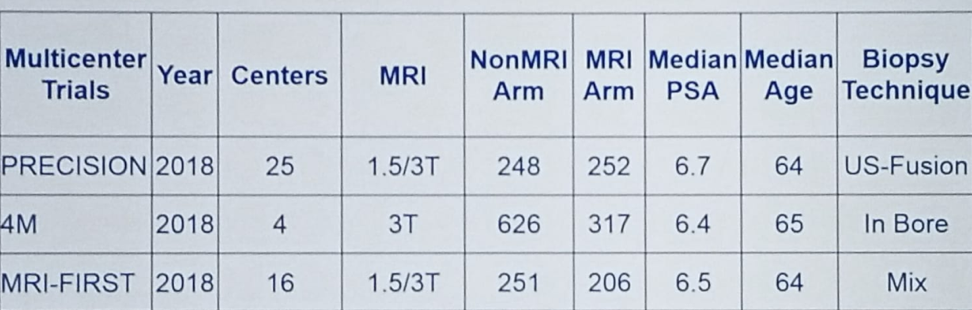
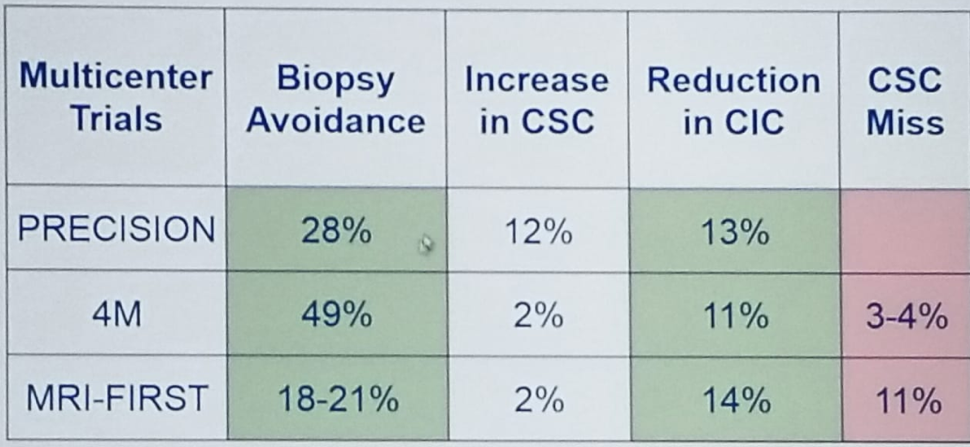
Figure 1 - Latest European Multicenter Randomized Controlled Trials in Biopsy Naïve Men
In the current paradigm the risk stratification is heavily based on human interpretation and performance:
- The radiologist who provided MRI interpretation
- The urologist/radiologist who performed the biopsy
- The pathologist – who is responsible for the Gleason score and volume
Dr. Haier concluded his talk stating that there is also work and upgrades being currently performed to the PIRADS system used for diagnosis (version 2.1 and 3). This upgrade will include quality assurance, report templates, certification, standards for significant interval change in imaging, brain uptake of Gadolinium, biopsy qualification, and biparametric MRI. These anticipated changes and upgrades should, in theory, improve the diagnostic accuracy of mpMRI and make it less prone to errors.
Presented by: Masoom Haider, BAM, MD, FRCPC, Professor, Mi Research Lead - Radiomics/Quantitative Imaging, Toronto General Hospital, Dept of Medical Imaging, University of Toronto, Ontario
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter: @GoldbergHanan at the CUOS – Canadian Uro-Oncology Summit 2019, #CUOS19 January 10-12, 2019 Westin Harbour Castle, Toronto, Ontario, Canada
References:
1. Kasivisvanathan V. et al. NEJM 2018
2. van der Leest M. et al. European Urology 2018
3. Rouvière O. et al. Lancet Oncology 2019
4. Gronberg H et al. European Urology 2018
5. Stumpe, M (2018, November, 16). Improved Grading of Prostate Cancer Using Deep Learning [Blog post] Retrieved from https://ai.googleblog.com/2018/11/improved-grading-of-prostate-cancer.html


