Felix Couture, MD, started his presentation with a statement that in their clinical expeience despite using aforementioned nomograms and rigorous preoperative planning, NVB preservation techniques change intraoperatively. Reasons for these deviations can include challenging anatomical features, disrupted surgical planes during the procedure and other unexpected reasons making the resections technically challenging.
Authors performed a retrospective review of a prospectively maintained database of 578 patients undergoing RARP performed by a single surgeon (KZ). Side-specific (left and right) NVB preservation technique was planned preoperatively. Surgical techniques were either nerve-sparing (NS) or non-interfascial technique (NIFT) and partial extrafascial and wide extrafascial techniques. Preoperative plans were compared to final technique used in RARP. Patient speficic analysis was performed to identify predictors of deviation in surgical technique among selevted variables including: age, BMI, PSA, Gleason score, tumor stage, prostate volume, number of lifetime biopsies, time from biopsy to RARP, history of post biopsy sepsis, preoperative SHIM score.
Prostate side-specific analysis was also done and also include side-specific variables: laterality, maximum percentage of disease in ipsilateral core biopsies, total number of ipsilateral positive core biopsies and ipsilateral ECE on final pathology. Multivariate logistic regression models were generated to identify any significant predictors. Authors also analyzed functional outcomes including potency and continence as well as oncological outcomes such as PSM and BCR based on deviation in NVB preservation.
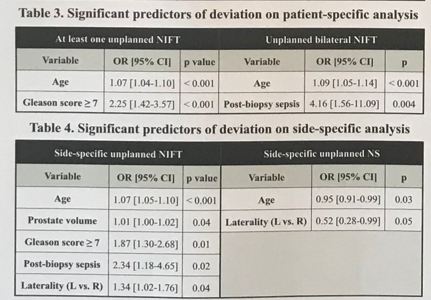
Dr. Couture reported that older age, Gleason score of >7, post-biopsy sepsis, larger prostate volume, and laterality significantly predicted more unplanned NIFT during RARP. As expected, unplanned NIFT was associated with poorer functional outcomes, with no impact on oncological outcomes (Figure 2). Primary goal of the RARP procedure remains to free the patient from malignant cells and in order to achieve this outcome, often deviations take place with subsequent consequences on functional outcomes.
Figure 1
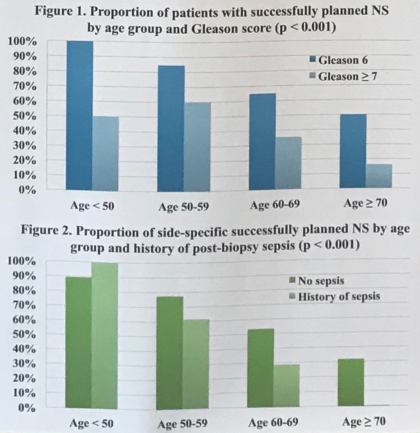
Figure 2
Kevi Zorn, MD, commented that the number of lifetime biopsies was not a predictor of unplanned NIFT, a novel and valuable finding for patients under active surveillance who have a concern that repeated biopsies can somehow impact the anatomical structures which potentially can influence surgical outcomes. Authors provide a new insight that should guide preoperative counselling and help set patient expectations with regards to functional outcomes.
Presented by: Felix Couture, MD
Co-Author: Kevin Zorn, MD
Written by: Zhamshid Okhunov, Twitter: @OkhunovZham, (Department of Urology, University of California-Irvine at the 73rd Canadian Urological Association Annual Meeting - June 23 - 26, 2018 - Halifax, Nova Scotia


