(UroToday.com) The 2024 American Urological Association (AUA) Annual Meeting held in San Antonio, TX between May 3rd and 6th, 2024 was host to an imaging/uroradiology poster session. Dr. Marcelo Bigarella presented the interim analysis of a phase II diagnostic trial assessing the impact of 18F-DCFPyL on the accuracy of mpMRI in men with low- and intermediate-risk prostate cancer.
PSMA-PET/CT is currently approved for the initial staging of patients with intermediate/high-risk disease and in the biochemically recurrent setting. There has been increased interest in evaluating the diagnostic performance of PSMA-PET in the primary (i.e., diagnostic biopsy) setting. The PRIMARY trial has demonstrated that a combined mpMRI + PSMA-PET/CT approach improves the sensitivity for diagnosing clinically significant prostate cancer from 83% to 97%, while reducing the false negative rate from 17% to 3.1%.1
To date, there is no study evaluating the clinical accuracy of PSMA-PET imaging in men with low- or intermediate-risk prostate cancer undergoing active surveillance. This is a phase II trial evaluating the diagnostic accuracy of 18F-DCFPyL PSMA PET combined with multiparametric MRI using a dedicated PET/MRI scanner and subsequent MRI/TRUS targeted biopsies. The target sample size is 100 men with very low, low, and intermediate-risk prostate cancer on active surveillance. Systematic and targeted MRI-US fusion biopsies (UroNav) were performed by an experienced urologist for all MRI PI-RADS ≥3 (standard of care) and research PET Likert≥3 lesion discordant on MRI (PI-RADS<3). Per lesion and per patient analyses were performed. The primary study outcome was the detection of clinically significant prostate cancer, defined as Grade Group ≥2 disease.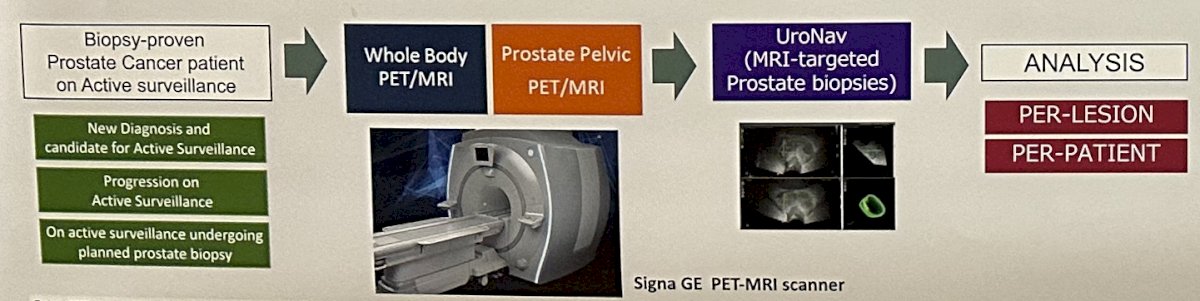
The baseline characteristics are summarized below. The median patient age was 68 years. The median PSA was 8.1, and the median prostate volume was 60.5 ml. Patients had been on active surveillance for a median of 25 months. The majority of patients (67%) had either very low or low-risk disease. A total of 163 lesions were biopsied. 123 PIRADS ≥3 lesions were identified on MRI (∼2.2/patient) with a mean lesion size of 11 mm. 80 Likert ≥3 lesions on PET (∼1.4/patient) were identified, with a mean SUVmax of 4.9.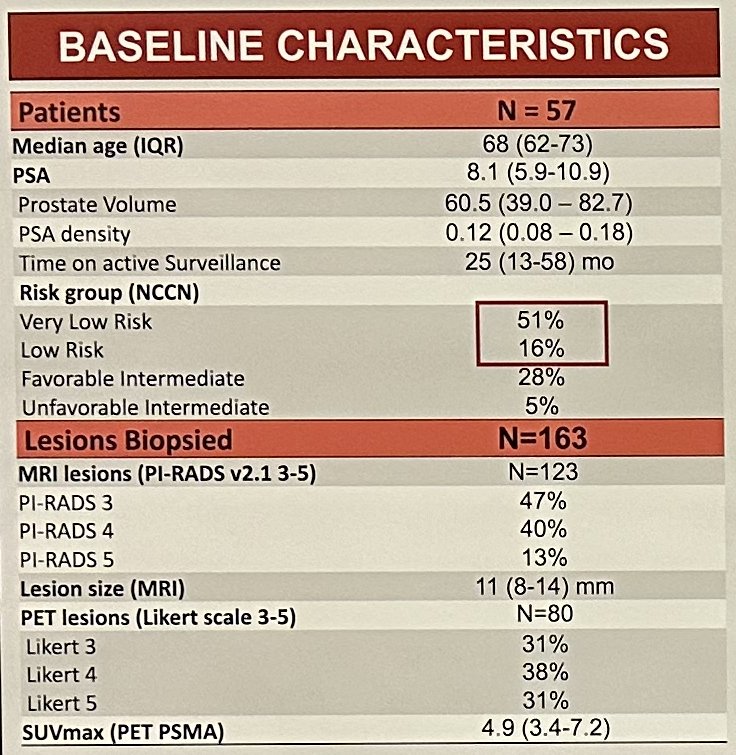
On study biopsy, clinically significant prostate cancer was found in 49% of men and in 22% of the targeted lesions. The SUVmax of prostate cancer lesions was positively correlated with the underlying grade (GG2, 3, and 5 were 4.2, 8.2, and 11.1, respectively).
The negative predictive value, sensitivity, and accuracy of mpMRI (PI-RADS ≥3) for clinically significant prostate cancer were 93%, 92%, and 43%, respectively. The addition of PSMA-PET to MRI improved specificity from 29% to 87%, with sensitivity decreasing from 92% to 58%. Overall, the accuracy improved from 43% to 80%. The addition of PET PSMA detected clinically significant prostate cancer in an additional 3/28 patients (11%). Avoiding biopsy of PI-RADS ≤3, Likert ≤3 lesions would have not missed clinically significant disease and would have saved 4/39 (10%) of the patients and 30/107 (28%) lesions from an unnecessary biopsy.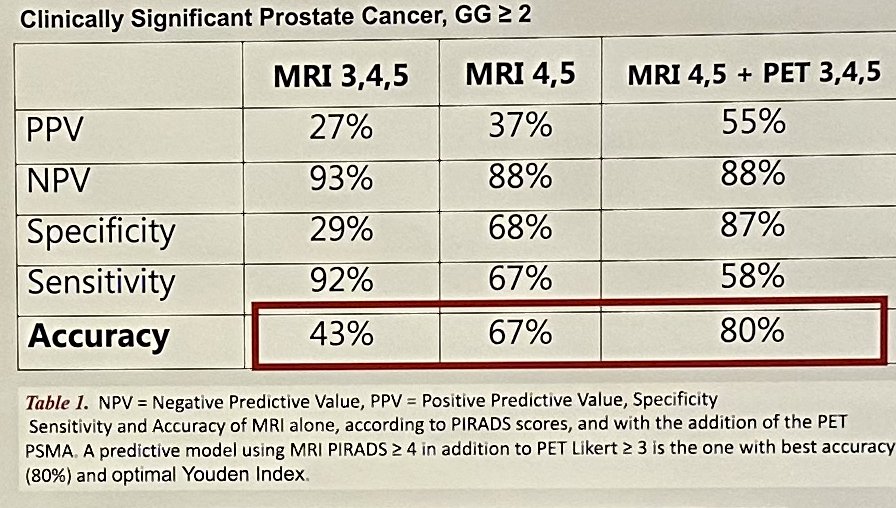
Dr. Bigarella and colleagues concluded that in this interim analysis, the addition of PSMA PET to prostate mpMRI improved the accuracy of clinically significant prostate cancer detection in men on active surveillance. Imaging and clinical predictive models including PSMA PET with mpMRI may identify men who could safely avoid prostate biopsy and coincident morbidity, as well as increasing the detection rates of clinically significant prostate cancer missed by MRI-biopsy alone.
Presented by: Marcelo Bigarella, MD, Urologic Oncology Fellow, Department of Urology, University of Wisconsin, Madison, WI
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024
References:


