(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX was host to the advanced kidney cancer podium session (PD18). Dr. Daniel Shapiro presented the results of a multicentric study using retrospective data from a cohort of patients with synchronous metastatic renal cell carcinoma (mRCC) treated with pre-surgical systemic therapy followed by cytoreductive nephrectomy. The primary endpoint of the study was to establish prognostic factors associated with overall survival, including radiographic response in the primary tumor and metastatic sites.
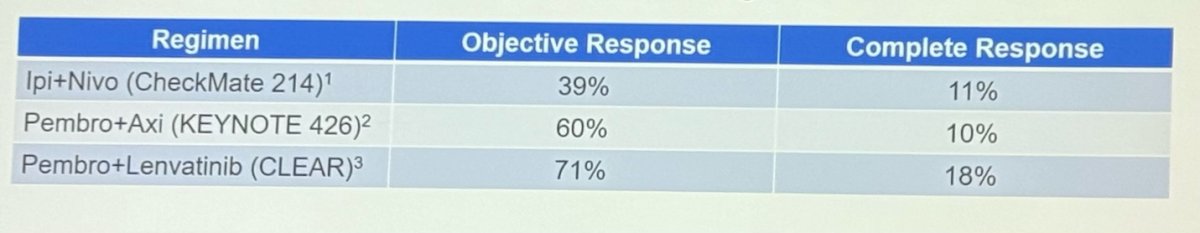
Dr. Shapiro began his presentation by highlighting the observed enhanced overall response rates with the availability of immunotherapy (IO) or IO + targeted therapy combinations as first-line systemic treatments for mRCC (Table below). However, a clinical dilemma remains in determining which patients with mRCC treated with upfront systemic therapy may benefit from cytoreductive nephrectomy (CN), and how we can identify more reliable predictors of survival to enhance our treatment decision-making for CN.
The objectives of the study were to determine the tumor response to targeted therapy versus IO among patients undergoing deferred CN and evaluating tumor response as a prognostic factor for OS among patients undergoing pre-surgical therapy and CN.
He went on to explain this study use data from five different institutions from 2010-2023. Primary tumors and metastatic sites were measured before the start of systemic therapy and prior to CN and were assessed per RECIST V 1.1 criteria. The patients were grouped according to the type of pre-surgical systemic therapy: targeted therapy (TT) vs Immunotherapy (IO). Tumor measurements included maximum primary tumor (PT) diameter, sum of metastatic tumor diameters, and sum of PT+ metastatic sites diameters.
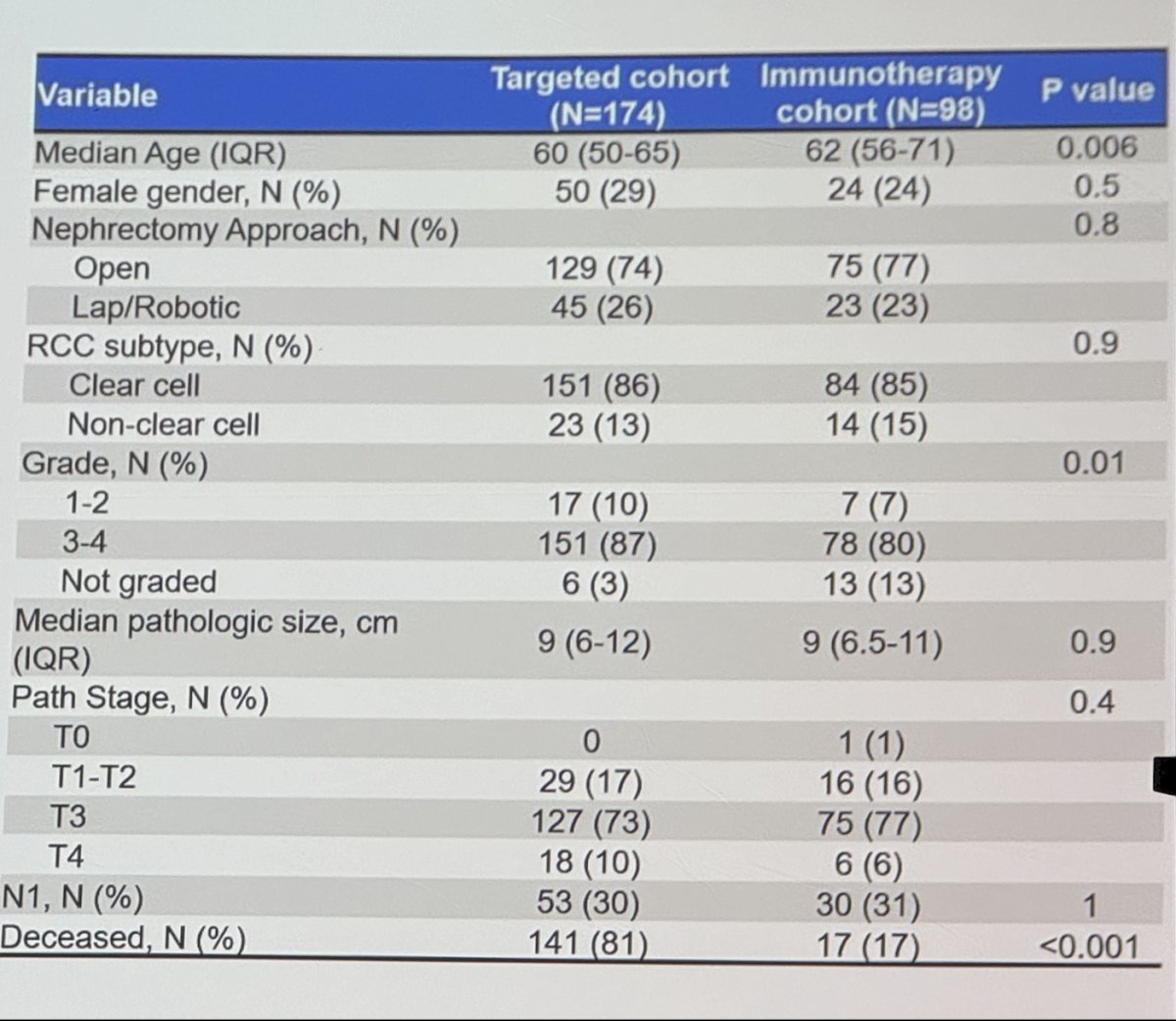
This analysis included 272 patients treated with systemic therapy before CN. Of these 174, received TT and 98 received IO. The median time from systemic therapy to CN was 5 months and the median follow-up was 51 months. Clinical characteristics before systemic therapy were similar between targeted therapy and IO groups. The median PT diameter was 9 vs. 9.3 cm, total metastatic burden 5.2 vs 5.6 cm, and PT+metastatic burden 14.4 vs 16 cm (p>0.05).
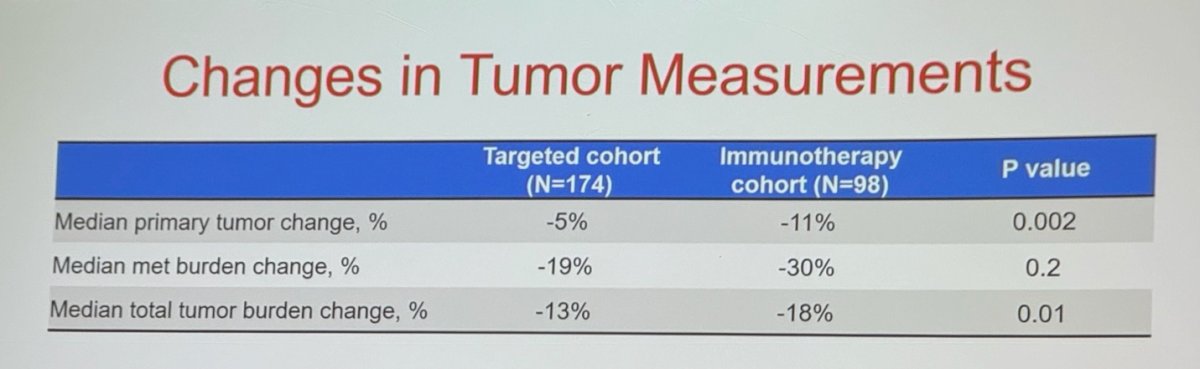
Pre-surgical IO treated patients had greater PT+metastatic burden reduction vs targeted therapy (median 18% vs 13%, p=0.01). a higher proportion of pre-surgical IO patients achieved a partial response per RECIST criteria (34% vs 19%, p=0.01).
Regarding overall survival (OS), patients treated with preoperative IO demonstrated significantly improved OS compared to those treated with targeted therapy (p<0.0001).
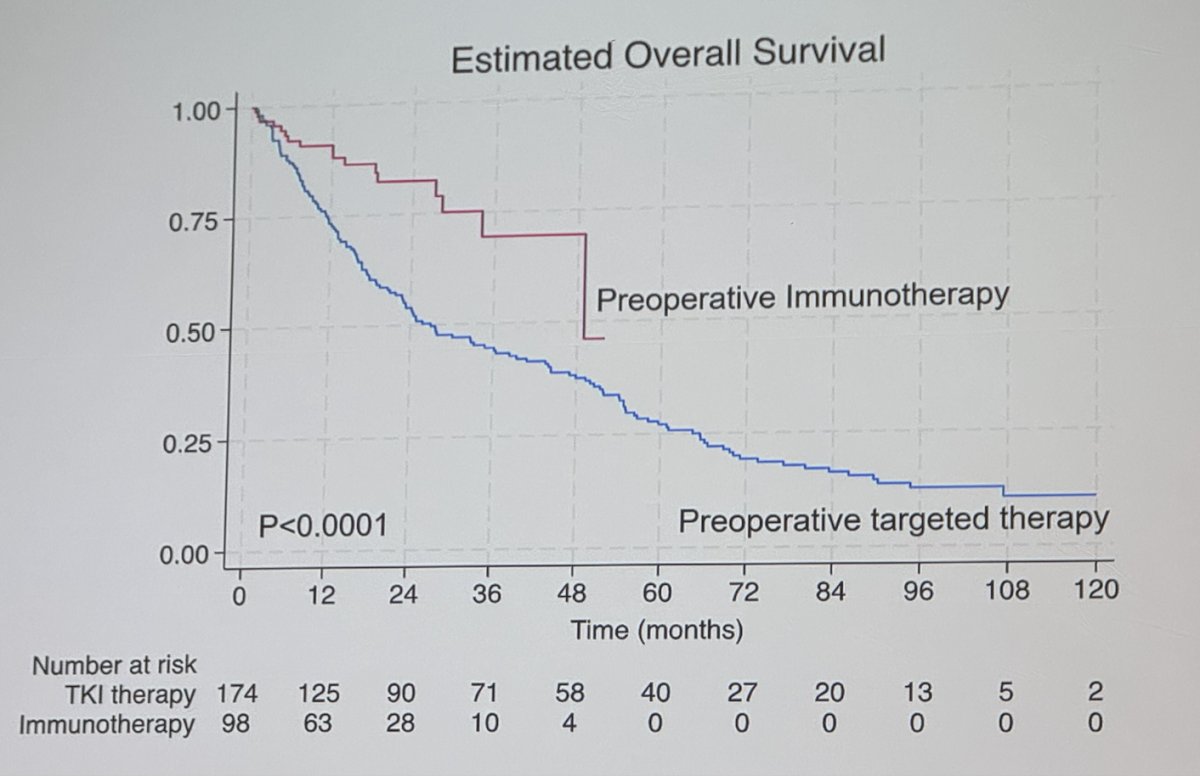
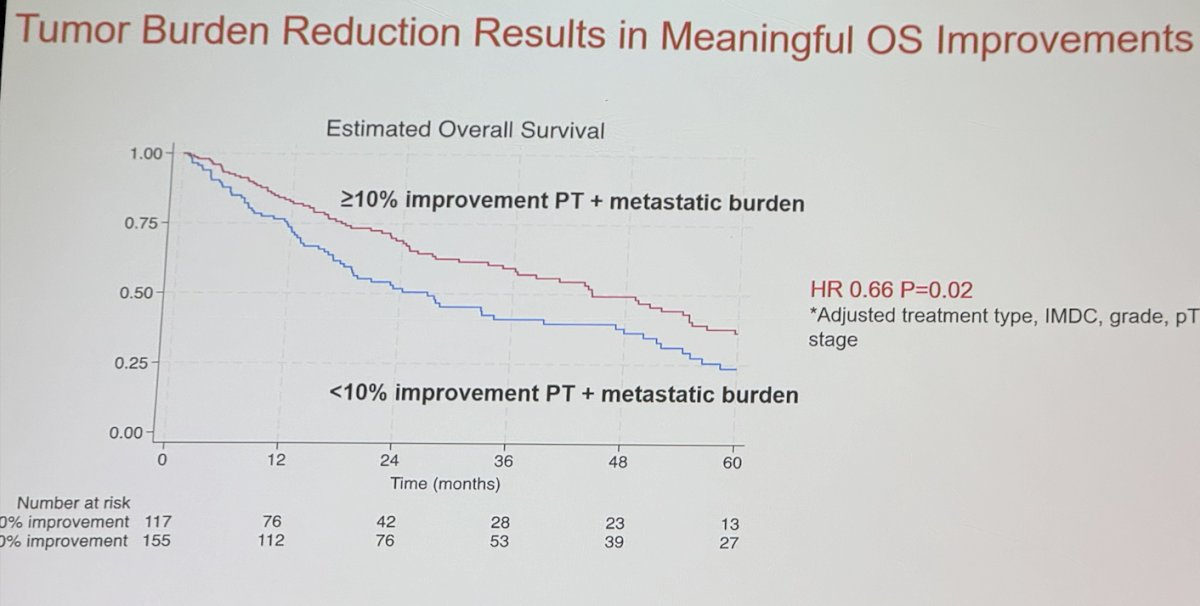
The investigators used multivariable analysis adjusting for pre-surgical systemic therapy type (TT vs. IO), IMDC risk group, WHO/ISUP grade and pathological stage. On multivariable analysis ≥10% total PT+metastatic size reduction was significantly and independently associated with improved OS (HR 0.66, p=0.02).
Dr Shapiro concluded:
- In their multicenter retrospective cohort, patients with mRCC treated with upfront systemic therapy followed by CN, IO therapy was associated with greater tumor size reduction per RECIST and improved OS.
- Achieving a ≥10% decrease in total tumor burden (primary tumor + metastatic sites) was prognostic for improved survival following CN. This size threshold could be used to improve patient selection for CN after systemic therapy.
Presented by: Daniel Shapiro, MD, Urologic Oncologist at University of Wisconsin-Madison
Written by: Julian Chavarriaga, MD – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


