(UroToday.com) In this first plenary session of AUA 2023, Dr. Rastinehead delivered a State of the Art Lecture on the Future of “Interventional Urology.” First, he kicked off with some background on the Current Status of Intervention Urology (an intersection of Interventional Radiology and Urology) and the history of the field.
In 2023, there is already an increasing integration of IR/GU into the field of Urology – including prostate MRI with fusion biopsy, renal tumor biopsy, renal embolization and renal ablation. But, there are definitely more areas that are up and coming in this area of overlap.
He notes that Collaboration is essential for progress and innovation – and will help improve care for our patients. He did ask for everyone to keep an open mind as the field moves forward!
From a historical perspective, he notes the following paradigm shift:
- Werner Forssmann performed the first cardiac catheterization (on himself!) in 1929 as a Cardiology trainee – but eventually became a Urologist. He was the first Urologist to earn a Nobel prize. By the 1960s, this became standard.
- 1980s – there was a shift to percutaneous/endoscopic treatment of stone surgery from open surgery.
- 1990s – there was a paradigm shift to laparoscopic surgery from open surgery (Kavoussi, Clayman and colleagues)
- 2000s – there was a paradigm shift to robotic surgery (Mani Menon and colleagues)
As for Uroradiology, he specifically noted the impact of Howard Pollack, MD who completed both a Urology residency (but had to leave due to hand injury) and Radiology residency – and then began the Division of Uroradiology at UPenn (1974). He founded the Society of UroRadiology and helped invent the endorectal coil that was critical for bringing mpMRI of the prostate to the forefront.
As he then noted, despite imaging advancements, better understanding of the biology of disease, and integration of new therapies, we have continued to maintain our own silos of practice (medical oncology, urology, interventional radiology, radiology), instead of integrating better. This is where there is a potential role for interventional urologists – similar to interventional cardiologists, nephrologists, etc.
* BUT, he does note that this would require hybrid training. He himself completed a Urology residency, an Interventional Radiology fellowship, and an SUO Urologic Oncology fellowship. In the future, hopefully, there will be a more integrated training pathway for those interested.
Looking at Interventional Urology now and in the future: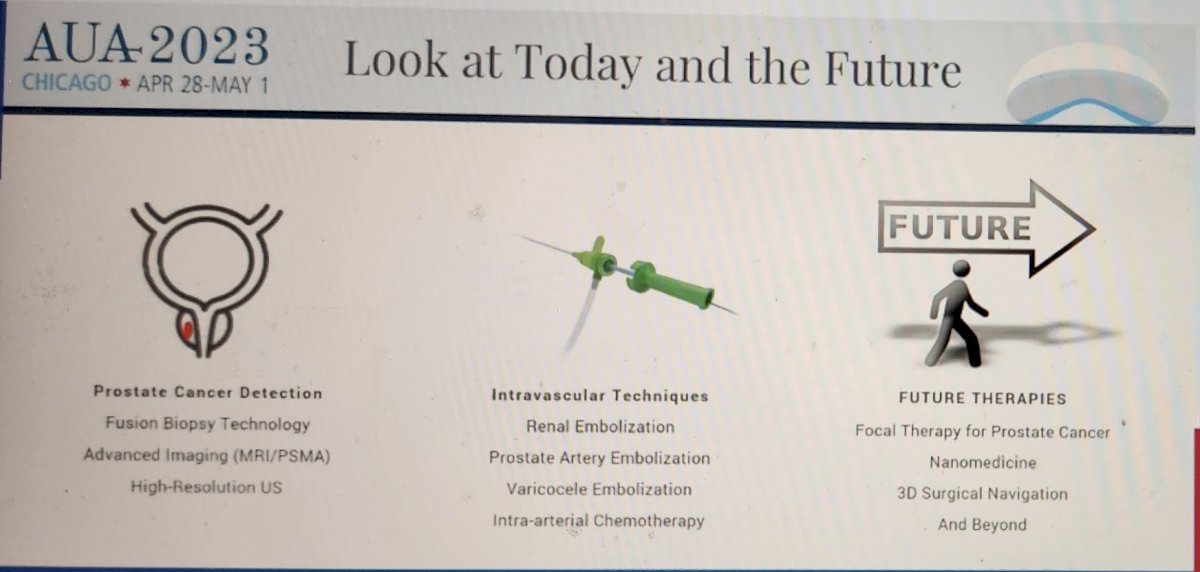
Prostate cancer detection, with better imaging (mpMRI) which has enabled better detection of clinically significant prostate cancer (fusion biopsy technology), has already become an established part of Urology practice.
Similarly, intravascular techniques for renal artery embolization, renal mass ablation, and varicocele embolization (especially outside the US), have clearly established roles within the current Urology paradigms.
However, there are newer uses that are being evaluated. He notes that PAE, which isn’t always accepted by most urologists, has increased data to support its use – as long as its done by someone experienced and with a good understanding of pelvic vasculature.
But, the future lies in the following:
- Focal therapy for prostate cancer – especially as the technology improves to not only identify significant lesions and guide the therapy but also to evaluate for therapy success (real-time).
- Modular operating rooms (similar to CVIR) allow for the use of 3D navigation/fusion, cross-sectional imaging, patient data tracking, and radiation safety to treat kidney stones, renal mass biopsies, and tube placement.
In order to accommodate these changes, we may have to incorporate changes to the training pathways (for those interested) to include:
- Imaging Rotations
- Rotations through Interventional Radiology
This can be either in residency training or incorporated into established fellowships (Endourology, SUO Urologic Oncology) or dedicated Interventional Urology fellowships.
At the end of the talk, in the interactive session, when the audience was asked whether Urology was ready for Interventional Urology, 64% said yes – and only 8% said we should leave it to others. This is promising!
We, as a field, have led the paradigm shift in many aspects of surgery and medicine (cystoscopy in 1877, TURP 1930, percutaneous stone surgery in the 1980s, laparoscopy in the 1990s, robotic surgery in the 2000s) – and this may be the next paradigm shift.
Presented by: Art A. Rastinehad, DO- Smith Institute For Urology At Lenox Hill
Written by: Thenappan (Thenu) Chandrasekar, MD – Urologic Oncologist, Associate Professor of Urology, University of California, Davis @tchandra_uromd @UCDavisUrology on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023


