(UroToday.com) The 2023 AUA annual meeting included the Bladder Cancer Forum, featuring a debate discussing surveillance and treatment challenges of intermediate risk non-muscle invasive bladder cancer (NMIBC). Dr. Stephen Williams started this session by highlighting a case of a 67 male with a history of gross hematuria for six months with no work-up during that time period.
He had no significant medical or surgical history but did have a history of smoking one pack per day for 20 years. He subsequently had a CT urogram that showed a filling defect in the posterolateral bladder wall with a suspected 1.5 cm bladder tumor. TURBT of this lesion demonstrated a 3 cm Ta low grade tumor on a stalk, as well as an additional 1 cm Ta low grade tumor that was resected:
There was no CIS in the specimen and muscle was present, but not involved.
Dr. Paolo Gontero then made the case for treatment in this particular patient. He noted that according to the EAU risk stratification, intermediate risk is defined as patients without CIS who are not included in the low, high, or very high risk groups, whereas the IBCG defines intermediate risk as multifocal low grade or recurrent low grade. He notes that if this patient were Ta high grade, these patients have similar outcomes to other intermediate risk non-muscle invasive bladder cancer. Furthermore, intermediate risk disease has a 10-year probability of progression of 8.5%, which is not that much lower than patients with high-risk disease (14%). Additionally, if this patient had his information added to the EORTC bladder cancer recurrence and progression calculator, Dr. Gontero notes that he would have a 31% risk of progression at 5-years and 15% at 1-year.
With regards to the data for BCG, an individual patient data meta-analysis from 2009 assessing 2,820 patients (74% intermediate risk disease) with a median follow-up of 4.4 years showed that BCG maintenance was associated with a 32% risk of reduction in recurrence.1 There was no significant difference in progression and survival. Additionally, BCG with maintenance was better than Mitomycin C, but was associated with more side-effects:

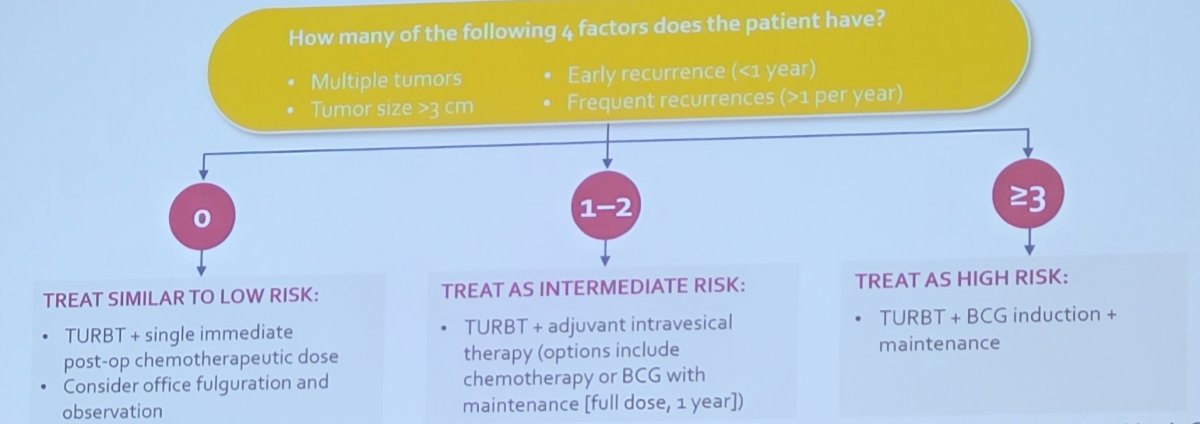
Recent work from the International Bladder Cancer Group has provided updated definitions and management recommendations for the treatment of intermediate risk non-muscle invasive bladder cancer.2 Among intermediate risk (low-grade tumors), the following risk factors should be assessed:
- Tumor size >3 cm
- Multiple tumors
- Early recurrence (<1 year)
- Frequent recurrence (>1/year)
- Failure of previous intravesical treatment
For those patients with none of the above risk factors, they should be treated similarly to those with low-risk disease (no additional treatment). For patients with 1-2 risk factors, they should be treated as intermediate risk disease and thus treated with additional adjuvant induction intravesical chemotherapy (or BCG if prior chemotherapy has been used). For patients with >= 3 risk factors, they should be treated as high risk disease with BCG/chemotherapy for at least 1 year, with maintenance therapy:
Dr. Gontero notes that active surveillance is not adequate for non-muscle invasive disease. There is poorly defined inclusion criteria (T1? High-grade?), the schedule and type of surveillance is to be determined (patients prefer an intense follow-up schedule), there is a high failure rate (50% at 1 year), and there is a lack of pathological correlation with visual assessment (cystoscopy) in defining active surveillance failure (in 30% of cases there is no pathological findings of bladder cancer), thus pathological proof cannot be avoided in active surveillance. However, perhaps we can reduce the burden of TURBT in recurrent intermediate risk bladder cancer, as laser fulguration has recently been shown to be as good as TURBT, with lower complications, and better quality of life. Additionally, intense follow-up is likely unnecessary as patients followed every six months for one year followed by annual thereafter have been shown to do just as well as patients with more intense follow-up: no difference in recurrence, progression or cancer specific survival, with 2/3 reduction in necessary follow-up visits.
Dr. Gontero concluded his portion of the debate in favor of treatment for this patient with the following conclusions:
- Intermediate risk non-muscle invasive bladder cancer is not always indolent, which highlights the importance of risk stratification
- Progression cannot be overlooked and pathology must be determined
- Any available treatment must be attempted in order to try to impact the natural history
- Active surveillance is not yet mature
- The burden of TURBT can be reduced while maintaining the advantages of surgery (tumor ablation and pathology)
- Follow-up does not need to be intense, but should be long term
Dr. Gary Steinberg then took the position of surveillance for this patient. He notes that the goals of surveillance are to diagnose bladder cancer early before the development of invasive disease. However, there are several issues:
- The bladder cancer diathesis is variable with regards to progression from non-muscle to muscle-invasive disease
- Surveillance is invasive, time consuming, and expensive
- Early detection of Ta low grade may not matter and it is unlikely to lead to progression
- Can we eliminate cystoscopy?
- Can we detect genetic changes?
With regards to non-muscle invasive bladder cancer, Dr. Steinberg notes that complete resection of all tumor is the standard of care. However, should we be doing adjuvant therapy for all patients? Immediate peri-TURBT intravesical chemotherapy is thought to eliminate implantation of tumor cells, with randomized studies showing an 11.7% decrease in recurrence rate using a single post-TURBT dose of chemotherapy (mitomycin C, gemcitabine, doxyrubicin, epirubicin). Low grade primary and solitary tumors are low risk and benefit the most from surveillance, with decreased recurrence rates of 12-24 months with blue light cystoscopy with Cysview. There are several outstanding questions regarding how effective we are with treating intermediate risk disease:
- What is the benefit of intravesical therapy?
- Is surveillance or watchful waiting harmful?
- Is the risk of progression or cancer specific survival different?
- Is low grade non-muscle invasive bladder cancer the same as high grade?
- Risk of progression is critical to understand
Dr. Steinberg highlighted that historical reports suggest that the recurrence risk is 5-10% for low grade Ta, 15-40% for high grade Ta, and 30-50% for T1 high grade. The following shows the estimated recurrence and progression rates for each AUA NMIBC risk category at 6, 12, and 24 months based on adjuvant treatment received:

TURBTs for intermediate risk disease require anesthesia, which can be problematic for older patients, sicker patients, and those on anticoagulants. These procedures can be associated with complications, such as pain and urinary symptoms, bleeding, infection, and injury (including perforation). A study assessing outcomes of TURBT showed that 30 day complication rates were 5.1%, with readmission rates of 3.7%, similar to major urologic oncology cases.3 Additionally, there was a decline in health-related quality of life over time, as well as financial toxicity associated with non-muscle invasive bladder cancer treatment.
Dr. Steinberg notes that his surveillance schedule is as follows:
- Low-risk: cystoscopy at 3 months, if negative, cystoscopy at 1 year and then annually for 5 years
- Intermediate risk: customized between low and high-risk schedules
Ultimately, the 3 and 6 month cystoscopy is critical.
Dr. Steinberg concluded his presentation in support of surveillance in this patient with the following take-home messages:
- Intermediate risk non-muscle invasive bladder cancer is heterogeneous and associated with high rates of recurrence, but low rates of progression and cancer specific mortality
- Current clinical guidelines vary, with the AUA and SUO recommending limiting intravesical BCG to those with high grade disease secondary to BCG shortages
- Current intravesical chemotherapy is limited in long-term efficacy
- Watchful waiting surveillance with fulguration in clinic with local anesthesia is preferential
- New treatment options with chemoablation and novel intravesical therapy delivery are currently being studied
Moderator: Stephen B. Williams, MD, MS, FACS, University of Texas Medical Branch, Galveston, TX
Debater: Paolo Gontero, MD, San Giovanni Battista Hospital, Torino, Italy
Debater: Gary D. Steinberg, MD, NYU Langone Health, New York, NY
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
References:
- Malstrom PU, Sylvester RJ, Crawford DE, et al. An individual patient data meta-analysis of the long-term outcome of randomized studies comparing intravesical mitomycin C versus bacillus Calmette-Guerin for non-muscle invasive bladder cancer. Eur Urol 2009 Aug;56(2):247-256.
- Tan WS, Steinberg G, Witjes JA, et al. Intermediate-risk non-muscle invasive bladder cancer: Updated Consensus Definition and Management Recommendations from the International Bladder Cancer Group. Eur Urol Onc. 2022 Oct;5(5):505-516.
- Pereira JF, Pareek G, Mueller-Leonhard C, et al. The perioperative morbidity of transurethral resection of bladder tumor: Implications for quality improvement. Urology. 2019;125:131-137.


