As the authors of this abstract note, clear cell renal cell carcinoma (ccRCC), the most common histologic subtype of RCC, is known to have aggressive histology with metastatic potential. A clear cell likelihood score (ccLS) based on multiparametric magnetic resonance imaging (mpMRI) has shown reasonable accuracy in identifying ccRCC in a retrospective cohort. In this abstract, the authors now report the diagnostic performance of ccLS to predict ccRCC in a prospective cohort of renal mass patients.
The authors assessed patients with a known renal mass who underwent mpMRI at their institution between June 2016 and April 2018. Patients were then assigned a ccLS in the clinical mpMRI report. They then retrospective identified all patients with available pathological tissue diagnosis (biopsy or surgery). ccLS was reported based on the likelihood of ccRCC histology using a previously reported Likert interpretation algorithm - a ccLS score of 4 or 5 was considered positive for ccRCC pathology and 1 or 2 considered negative. Lesions were grouped according to clinical stage (cT1a, cT1b, cT2-4) and confusion matrix analysis was performed.
245 patients (mean age 60 ± 13 years) with 256 renal masses were identified. Complete demographics info is below:
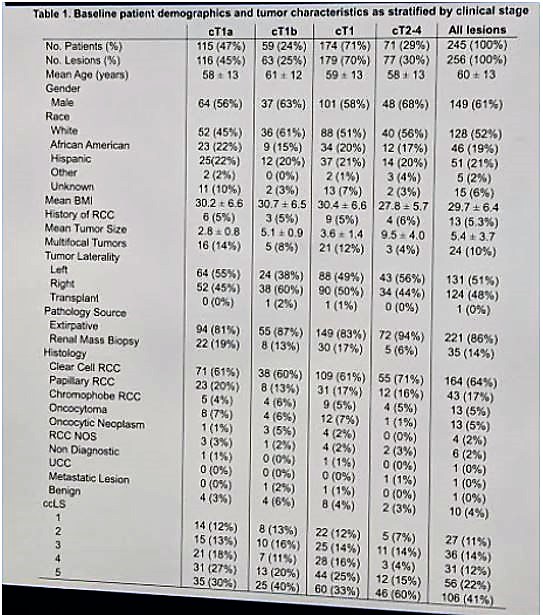
Mean tumor size was 5.4 ± 3.7 cm.
It should be noted that only 64% of lesions were ccRCC – the rest included 17% papillary RCC (type not specified), chromophobe RCC (5%) and others (less frequent).
Their take-home table of results is below:
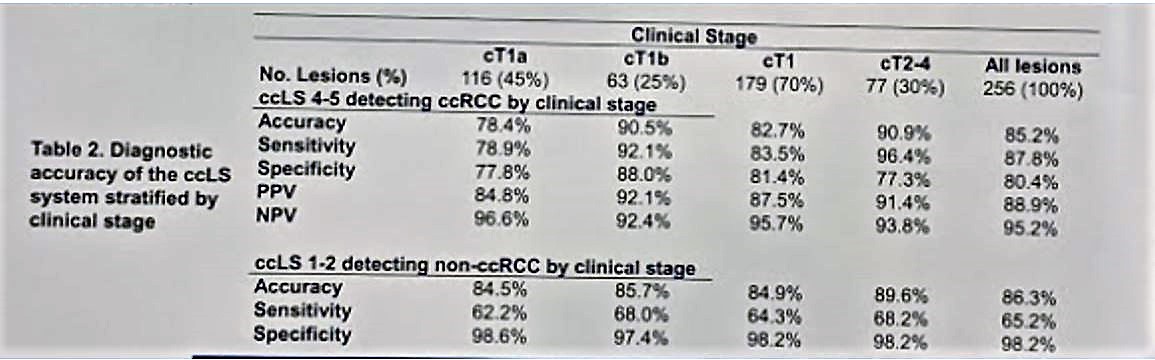
When stratified by the clinical stage of the mass, the diagnostic ability of ccLS improved as the clinical stage increased (Table above).
Notably, a ccLS of 1 or 2 had a 98.2% specificity for all cT1 lesions – which means that for small masses with ccLS of 1-2, ccRCC can effectively be ruled out. On the other hand, a ccLS score of 4-5 in a cT2-4 mass is very likely to be ccRCC - they had a 93.8% specificity in cT2-4 tumors.
Using this information, the authors suggest that mpMRI can reasonably identify ccRCC histology in renal masses of all sizes with improved performance in higher stage lesions. A renal mass biopsy can be omitted in larger or more advanced ccLS 4-5 lesions. They also suggest active surveillance (AS) in smaller masses with low ccLS. It is the patient population in the middle that may benefit from a renal tumor biopsy.
However, my one concern with this study is that it only discriminates for ccRCC – and assumes all other histologies are benign/indolent. Yet, there is no separation of the 17% of patients with papillary RCC into type 1 or 2 – and so, ccLS does not adequately predict aggressive histology. It only predicts ccLS. I do think it's beneficial in patients with larger tumors and high ccLS. But AS should be used with caution in patients with smaller masses and low ccLS – as aggressive non-ccRCC variants may still be present.
Presented by: Ryan Steinberg, MD, University of Texas Southwestern, Dallas, Texas
Written by: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University @tchandra_uromd, @JEFFUrology at American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


