Using a provincial cancer registry in Ontario, Canada, the authors from the University of Toronto, aimed to investigate trends in diagnosis and initial management of localized PC at the population level within the province of Ontario. This is taken with the caveat that practice patterns and guidelines are slightly different in Canada than they are in the United States – while most Canadian guidelines follow their US counterpart, there are nuances to the healthcare system that may favor certain management patterns over others.
In this study, the authors focused on localized PCa diagnoses between January 2011 and October 2016 – all patients in Ontario are captured with this provincial database, providing for an in-depth analysis of localized PCa in a large population comparable to a United States region. Cases were then linked to health-administrative databases to determine the proportion of patients undergoing either radical prostatectomy (RP), radiation therapy (RT), active surveillance (AS) or watchful waiting (WW). Furthermore, they determined the fraction of low-risk patients (based on D’Amico risk stratification) among each management modality. Data were aggregated at a monthly level and descriptively analyzed as time series – to help explore temporal relationships. Note that this time period overlaps the USPSTF 2012 recommendations against PSA screening – but does not account for the 2018 update for shared decision making re: PSA screening.
During the accrual windows of 70 months, 33,128 index cases were identified.
They detected a clear change in the slope of the linear trend in monthly PC incidence (Figure below): in the first month, it was 581 diagnoses; in the last month 482.
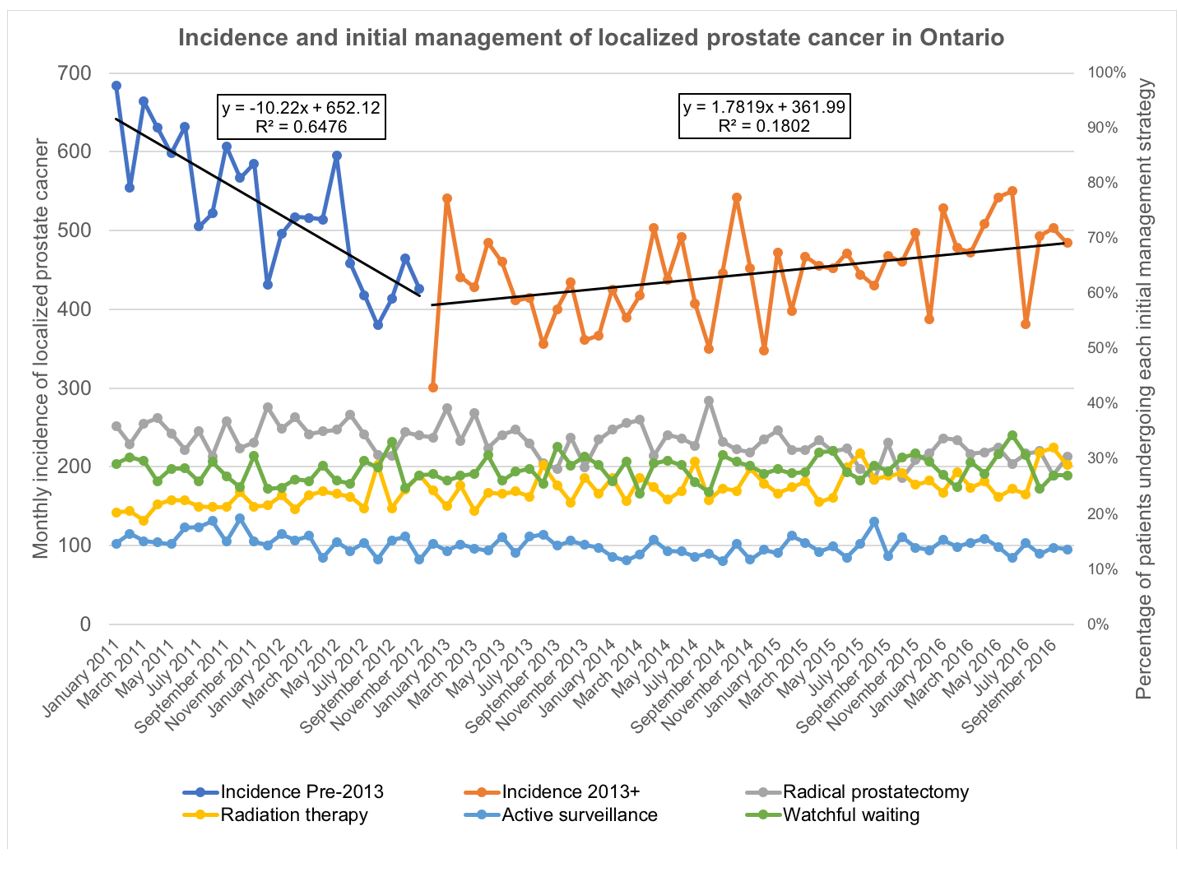
However, this is not a steady decline throughout the entire time period. It steadily declines until 2013, and then the incidence begins to rise. This may, in fact, be due to the change in the USPSTF recommendations.
The evaluation of the initial management strategies demonstrated a decrease in RP (34.8% to 30.8%), an increase in RT (21.4% to 26.5%) and a mostly stable proportion of patients initially undergoing AS or WW.
When specifically looking at low-risk patients, the fraction among the definitive treatments (RP and RT) steadily decreased since 2011 (RP: 18.1%; RT: 13.4%) and currently plateaus at a very low level (RP: 6.0%; RT: 2.7%). AS in the low-risk patients is observed in about ***% of patients.
Based on this information, the authors conclude the following:
- They identified a clear decrease in diagnosis that temporally aligns with the publication of the United States Preventive Services Task Force Recommendation in 2012 not to screen patients with the prostate-specific antigen test
- They further noticed an increase in RT at the cost of a decrease in RP
- In concordance with most of the current recommendations, most patients presenting with low-risk disease are spared from definitive treatment
Toronto, Ontario, Canada
SUBMITTED BY: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University, @tchandra_uromd, @JEFFUrology at American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


