Polyuria and overactive bladder were the most common types of urinary dysfunctions classified by analyzing full voiding charts. Some subjects were recommended medications, but less than half of these participants reported some improvement of their symptoms. These data were compared to patients who didn’t complete a voiding diary, and there was no significant difference in terms of improvement.
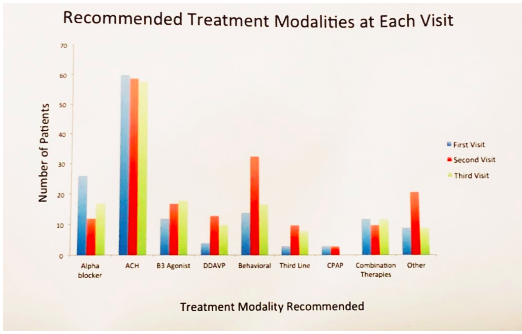
49% of new encounters were prescribed multifactorial treatment including behavioral modifications, medications, and referral to the sleep specialist to address probable underlying issues. However, only half of patients who were recommended multiple treatment options and decided to comply, have reported improvement of their symptoms. Although analysis of FVC revealed high percentage of patients with polyuria, desmopressin (DDAVP) was prescribed for mere 5% of patients (Figure 1).
This study is important because it can inform future researchers about shortcomings of currently available techniques. Results show that current diagnostic practices and available nocturia treatment options are not sufficient for improvement of patients’ symptoms and quality of life. FVC serves as a great tool, but its’ accuracy depends on patients compliance with completing a diary, and it’s not correlated with patient reported improvement. In terms of pharmaceutical treatments, DDAVP was rarely prescribed due to patients failing other therapies for the overactive bladder symptoms.
Presented by: Siri Drangsholt, MD, New York University School of Medicine, New York.
Co-authors: Maria Arcila Ruiz, MD; Victor Nitti, MD; Nirit Rosenblum, MD; Benjamin Brucker, MD
Written by: Hanna Stambakio, BS, Clinical Research Coordinator, Division of Urology, University of Pennsylvania Twitter: @PennUrology at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA
Watch a Video Presentation on this Study by Benjamin Brucker, MD


