(UroToday.com) The 2022 ASTRO annual meeting featured an improving prostate cancer survival session, including a presentation by Dr. Gregory Alexander discussing conditional survival of patients undergoing external-beam radiotherapy on RTOG 0126 and RTOG 0415. Patients with low- and intermediate-risk prostate cancer treated with radiation alone have excellent outcomes with anticipated long overall survival (OS). Although biochemical failure and OS rates are commonly reported from time of diagnosis, the relevance of such data diminishes over time for survivors. Conditional survival analyses can provide more relevant survival estimates for long-term survivors and help patients understand changing recurrence risks. The primary objective of this study presented by Dr. Alexander and colleagues was to report conditional OS and biochemical failure in patients with low- and intermediate-risk prostate cancer treated with radiation. A secondary objective was to determine if prognostic factors at initial treatment remain relevant later in survival.
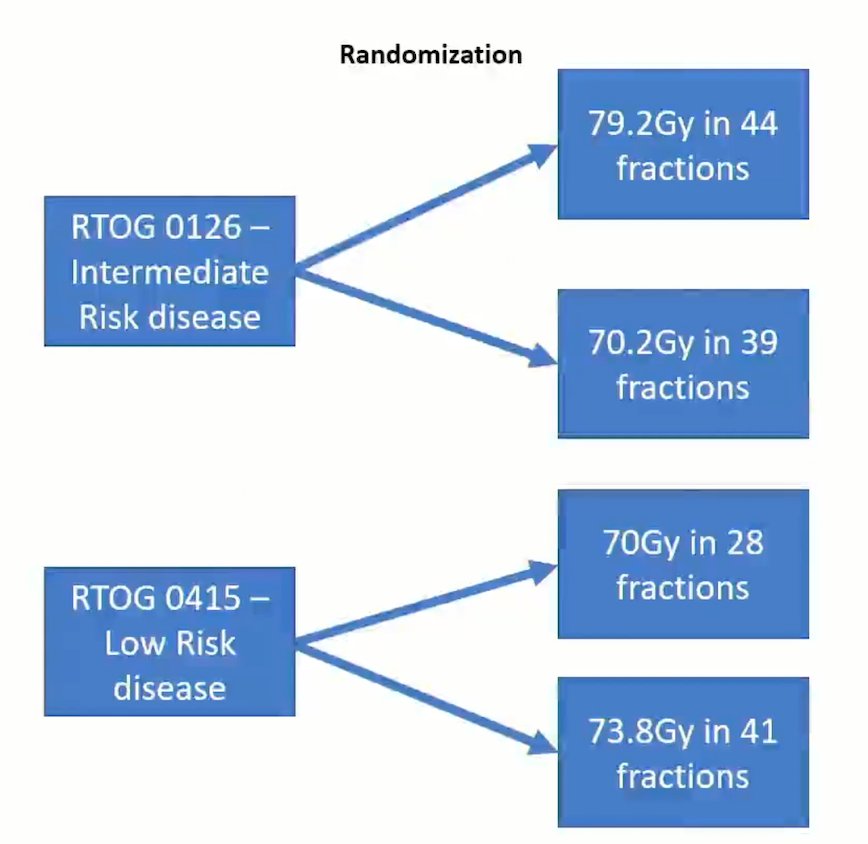
This study included a pooled analysis of patients with low- or intermediate- risk prostate cancer enrolled in RTOG 0126 or 0415 treated with radiation alone:
OS was calculated (Kaplan–Meier) at various survivorship time points. Cumulative incidence (Phoenix definition) was used to calculate biochemical failure rates. Risk factors (Gleason score, T stage, PSA, and EQD2 of prescribed dose) were analyzed at different time points using multivariable Cox proportional hazards modeling.
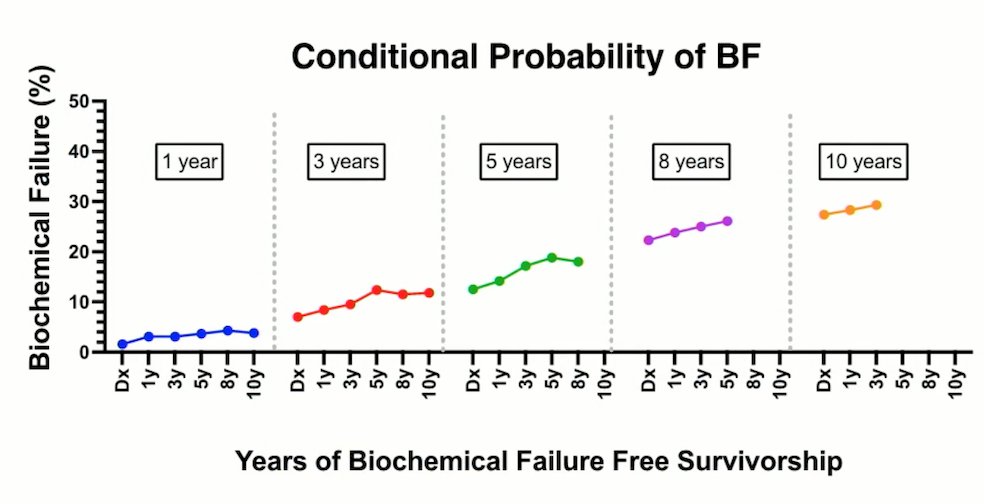
There was a total of 2,591 patients included (median age, 69 years of age; median PSA, 6.4 ng/mL; 48.5% with Gleason score 7; 34.2% with stage T2 disease), with a median follow-up of 6.9 years. The 3-, 5-, and 8-year rates of biochemical failure from time of treatment were 7.1%, 12.5%, and 22.3%, respectively. For patients surviving 1, 3, and 5 years without biochemical failure, the rates of biochemical failure in the next 5 years were 14.2%, 17.2%, and 18.8%, respectively:
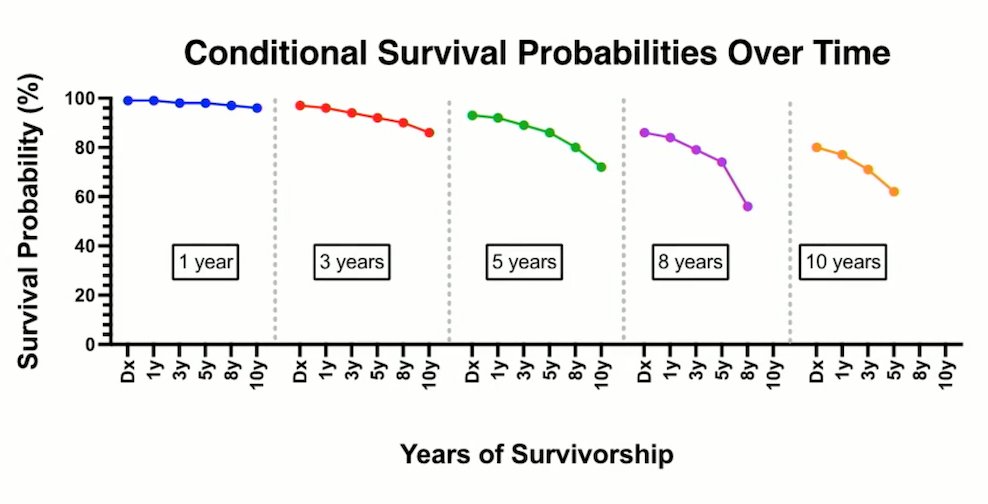
The 3-, 5-, and 8-year OS from time of treatment were 96.2%, 89.2%, and 41.0%, respectively. Patients with 1-, 3-, and 5-years of survival, had an additional 5-year survival rate of 73.3%, 42.6%, and 20.8%, respectively:
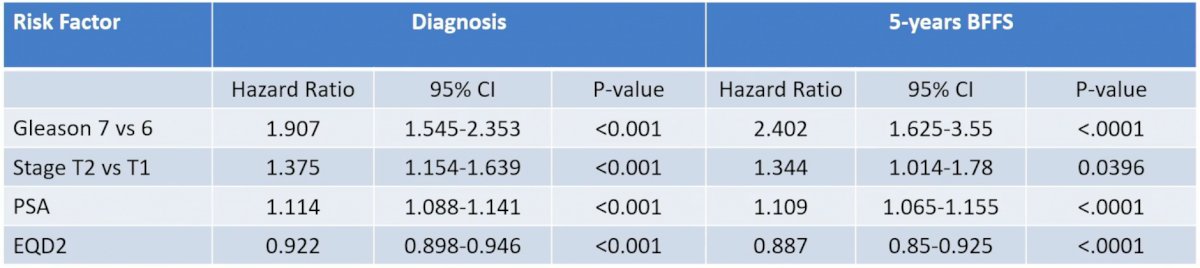
On multivariable analysis, Gleason score 7 (HR 1.907, p < 0.001), T2 disease (HR 1.375, p < 0.001), and increasing PSA (HR 1.114, p < 0.001) were significantly associated with increased risk of biochemical failure, whereas increasing EQD2 was associated with decreased biochemical failure rates (HR 0.922, p < 0.001). For patients who survived 5 years without biochemical failure, all initial prognostic factors remained statistically significant: Gleason score 7 (HR 2.402, p < 0.001), stage T2 (HR 1.344, p = 0.0396), PSA (HR 1.109, p < 0.001), and EQD2 (HR 0.887, p < 0.001):
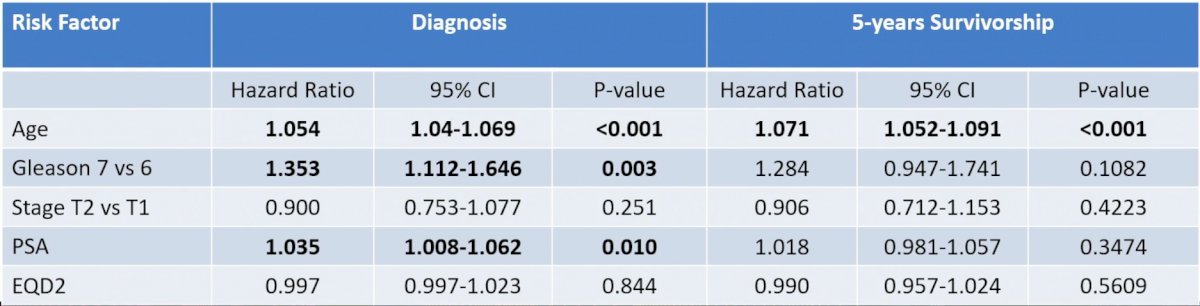
On multivariable analysis at diagnosis, Gleason score 7 (HR 1.353, p = 0.003), increasing age (HR 1.054, p < 0.001), and increasing PSA (HR 1.035, p = 0.01), were associated with all-cause mortality. For patients who survived 5 years, only age (HR 1.071, p < 0.001) was predictive of mortality:
Dr. Alexander concluded his presentation discussing the conditional survival of patients undergoing external-beam radiotherapy on RTOG 0126 and RTOG 0415 with the following take-home messages:
- Conditional risk of biochemical failure increases over time for patients with prostate cancer initially treated with radiation
- Initial biologic and treatment variables remain prognostic at long-term follow-up, with dose-escalated radiation continuing to be associated with decreased biochemical failure
- This data can be used to counsel patients for their risk of biochemical failure in follow-up and to help decide on the frequency of PSA monitoring
Presented by: Gregory S. Alexander, MD, Department of Radiation Oncology, University of Maryland Medical Center, Baltimore, MD
Co-Authors: R. F. Krc1, J. W. Assif2, K. Sun3, J. K. Molitoris4, Z. H. Rana2, P. T. Tran2, S. M. Bentzen3, and M. V. Mishra4; 1Department of Radiation Oncology, University of Maryland Medical Center, Baltimore, MD, 2Department of Radiation Oncology, University of Maryland School of Medicine, Baltimore, MD, 3Division of Biostatistics and Bioinformatics, University of Maryland Greenebaum Cancer Center, and Department of Epidemiology and Public Health, University of Maryland School of Medicine, Baltimore, MD, 4University of Maryland School of Medicine, Baltimore, MD
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


