(UroToday.com) In an interactive session of the American Society for Radiation Oncology (ASTRO) Annual Congress focussing on the management of patients with Intermediate Risk Prostate Cancer from initial consultation through treatment to follow-up, Dr. Michael Wan-Tien Chao presented on the role of rectal spacers.
Dr. Chao addressed a number of questions regarding the role of rectal spacers, beginning with the “What” of rectal spacing. These spacers are biomaterials that create a temporary separation between the prostate and rectum. The goal is to minimize the risk of rectal injury from prostate directed radiotherapy. With both dose escalation and aggressive hypofractionation, the risk of rectal injury may rise to lead to bleeding, mucus, diarrhea, and other more serious complications.
There are a number of different types of rectal spacers including hyaluronic acid (Barrigel), PEG hydrogel (SpaceOAR), biodegradable balloons, and biomaterials including blood or collagen. He focused on the first two of these.
Moving to the second question (“why”), Dr. Chao highlighted that, in the original hydrogel study, rectal spacing can improve baseline prostate to rectal separation from 2mm to 12mm. This results in a reduced mean rV70 by 73%. However, randomized data available to date is limited to conventional fractionation regimes with more contemporary trials using moderate hypofractionation to readout.

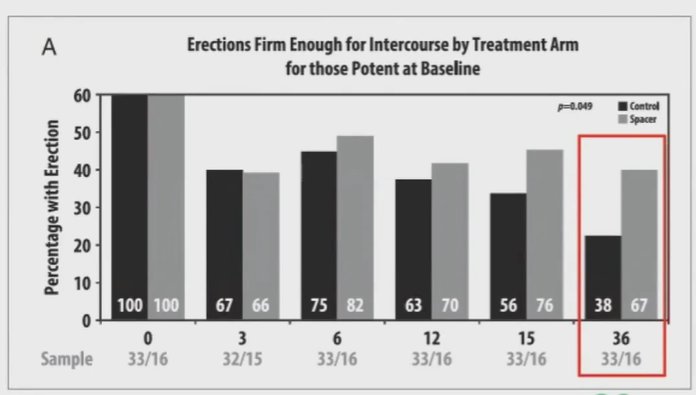
These changes led to a reduction in late grade 1 or greater GI toxicity from 9.2% to 2% and in late grade 2 or greater GI toxicity from 5.7% to 0%. Additionally, the use of the spacer improved patient-reported bowel-related quality of life at 3 years following treatment. While these benefits in GI toxicity were clearly demonstrated, there was no difference in rates of grade 2 or greater GU toxicity (7% vs 7%). However, rates of grade 1 or greater urinary incontinence were lower in patients who received the spacer (4%) compared to those in the control group (15%; p=0.046). This was manifest in the time from 20 months onward after treatment. Dr. Chao postulated that this may be due to decreased urinary irritation as a result of decreased rectal irritation. Additionally, this trial demonstrated that the use of a spacer was associated with improved long-term potency rates, with differences increasing over time.
Considering the clinical role for rectal spacing, Dr. Chao then laid out relevant eligibility criteria (the “who”) emphasizing that this is most suitable for patients with low to intermediate risk prostate cancer. While somewhat controversial, he suggested that it may also be appropriate for select high-risk patients with T1-2 disease based on MRI or selected patients with T3 disease in which the extracapsular extension is anteriorly or laterally located. The trials to date have been relatively conservative in their indications.
Dr. Chao highlighted that rectal spacing may be performed either in-office with local/regional anesthesia or in the operating room as a day procedure with general anesthesia. When considering performing rectal spacing under local anesthesia, he highlighted the importance of anesthetic infiltration of the subcutaneous perineal nerve for a saddle block, of a pudendal nerve block, or of a periapical triangular block.
Considering the logistics, Dr. Chao highlighted the importance of ceasing anti-coagulation prior to the procedure, of bowel preparation., and of prophylactic intravenous antibiotics. Biplanar trans-rectal ultrasonography is used for guiding the placement of the spacer, and gold seed fiducial markers if desired. Dr. Chao further uses a multi-purpose work-station including both a stabilizer and a stepper/cradle for the TRUS probe. Doing so allows both hands to be used for implantation.
The spacer is placed freehand under TRUS-imaging guidance into the peri-rectal space, the thin white line between the prostate and rectum.
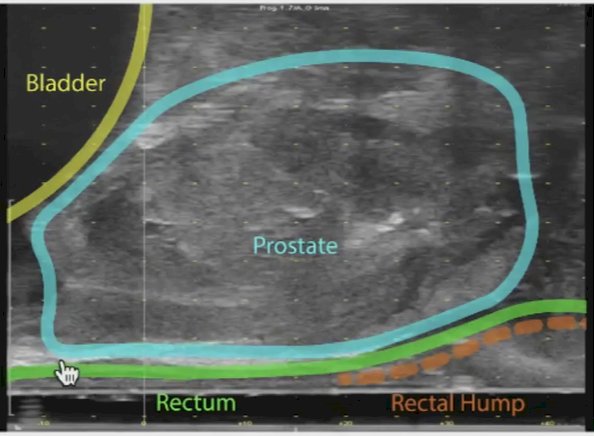
He emphasized that the rectal hump is well innervated so, for patients who are awake, it is key to avoid this by approaching from an initially anterior position. Under TRUS guidance, the needle is advanced to the mid-gland (if using hydrogel) or to the base (if using hyaluronic acid). Once the positioning is confirmed, hydro-dissection using saline can be performed prior to injection of the spacer. The spacer is then injected under direct guidance as the needle is withdrawn towards the apex. Correction can be made with the injection of an additional spacer agent for lateral asymmetry.
Dr. Chao further recommended the use of MRI for, in particular, the definition and delineation of the prostate apex and base. For those initially starting to use rectal spacers, he strongly emphasized the importance of obtaining MRI for quality adherence.
He then emphasized potential complications from the use of rectal spacers. Common side effects including pain and tenesmus are relatively mild. More rare complications may be more severe including infection, rectal wall infiltration, ulceration, abscess, fistula, and very rarely an allergic reaction to the agent.
Finally, Dr. Chao highlighted that hydrogel is stable for approximately three months and resorbed within 6 months. In contrast, hyaluronic acid is stable for up to 1 year and resorbed within 2 to 3 years. Thus, the timing of rectal spacing prior to the initiation of radiotherapy depends on the agent used. For patients using conventional fractionation among patients receiving hydrogel, this must be carefully timed given the 7 or more week treatment course.
In conclusion, he highlighted that rectal spacing can reduce rectal toxicity, improve bowel-related quality of life while minimizing urge incontinence and maintaining sexual potency. The role in patients receiving hypofractionated radiotherapy remains to be assessed in ongoing trials. Further, it is safe with relatively rare rates of severe complications.
Presented by: Michael Wan-Tien Chao, MBBS (Hons), AFRACMA, FRANZCR, Monash Health
Written by: Christopher J.D. Wallis, University of Toronto Twitter: @WallisCJD during the 2021 American Society for Radiation Oncology (ASTRO) Hybrid Annual Meeting, Sat, Oct 23 – Wed, Oct 27, 2021.


