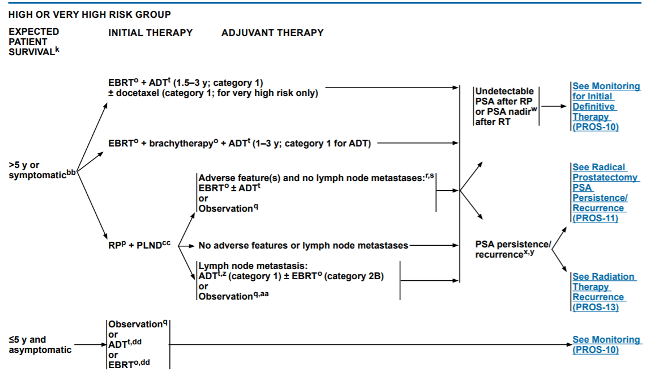
Dr. Moses began by highlighting the historical context for localized high-risk disease. Initially, there was hesitation to perform radical prostatectomy among these patients, so they often received, androgen deprivation monotherapy, radiotherapy, or combined radiotherapy and androgen deprivation therapy. Concerns regarding radical prostatectomy included positive surgical margins, the morbidity of surgery, and limitations of disease control through the omission of systemic therapy. However, as evidence as evolved, current NCCN now recommends three options including radical prostatectomy and pelvic lymphadenectomy, external beam radiotherapy with androgen deprivation therapy, or external beam radiotherapy plus brachytherapy with androgen deprivation therapy for patients with a life expectancy of at least five years.
This change from historical practice is predicated on a number of factors which Dr. Moses highlighted:
- Radical prostatectomy provides good, and durable, long-term cancer-specific survival, with reported rates of 85-95% at 10 years among patients with high-risk disease.
- In addition to cancer-specific survival, surgery is associated with durable local control.
- Surgery, as opposed to no local therapy or radiotherapy, can prevent local complications of high-risk and locally advanced prostate cancer including hematuria and lower urinary tract obstruction.
- Finally, pathologic examination of the prostate specimen provides important information which is both prognostic and may inform future treatments. In particular, radical prostatectomy allows for accurate pathologic staging (with approximately 60% of patients with high-risk disease undergoing surgery having organ-confined disease on final pathology) and pathologic grading (with previous work showing that nearly half of all patients with Gleason score 4+4 at the time of biopsy having down-grading at the time of prostatectomy).
For patients undergoing radical prostatectomy, the next question in their treatment is the role of postoperative radiotherapy. Dr. Moses highlighted existing guidelines from ASTRO.AUA which recommend adjuvant radiotherapy for patients with seminal vesicle invasion, extraprostatic extension, or positive surgical margins based on older randomized trials demonstrating a benefit in biochemical recurrence. However, this approach is not widely used, as he pointed out there are concerns of overtreatment and toxicity. Randomized data for the more commonly employed alternative, early salvage radiotherapy, has recently been presented demonstrating comparable if not better results to adjuvant radiotherapy while avoiding treatment for many.

Moving to considerations for patients treated with radiotherapy, instead of radical prostatectomy, Dr. Moses highlighted a number factors including the use of concurrent androgen deprivation therapy, combined external beam radiotherapy with brachytherapy, the use of whole pelvic radiotherapy, and the role of hypofractionation.
With respect to the use of concurrent ADT, Dr. Moses highlighted the seminal data from the EORTC trial led by Dr. Bolla demonstrating improved overall survival in patients receiving androgen deprivation therapy with radiotherapy, as compared to radiotherapy alone.

He further emphasized that existing data support the use of longer duration of androgen deprivation therapy (18-36 months).
With respect to the role of adding brachytherapy to external beam radiotherapy, he showed data from the ASCENDE-RT trial which showed no difference in overall survival for patients receiving combined therapy, despite some biochemical benefit. Further, patients receiving combined therapy had worse GU toxicity, patient-reported overall quality of life, patient-reported sexual function, and patient-reported urinary function.
Moving next to the role of whole pelvic radiotherapy, he highlighted data from GETUG-01 and NRG/RTOG 9413 which failed to demonstrate a benefit to this approach.

Finally, he discussed the role of hypofractionation, highlighting data from the HYPRO trial which demonstrated equivalent outcomes in the high-risk subgroup between hypofractionated and conventionally fractionated radiotherapy. Thus, this approach may reduce cost and patient burden while providing comparable results.
Dr. Moses then concluded by saying that patients with high-risk localized disease should be offered treatment with both surgery and radiotherapy backbones, acknowledging that multi-modality treatment is often required regardless of the choice of an initial local approach.
Presented by: Kelvin A. Moses, MD, Ph.D., Vanderbilt Health, Nashville, TN
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter at the ASCO20 Virtual Education Program, #ASCO20, August 8-10, 2020


