(UroToday.com) Neuroendocrine prostate cancer is an aggressive and heterogenous diagnosis which develops either de novo or in response to therapy during castration resistance, called “treatment-associated” or treatment emergent. These tumors can also be mixed, with simultaneous evidence of small cell and adenocarcinoma morphology. It remains a challenging disease with insufficient effective therapies. Dr. Richard Gagnon and colleagues endeavored to explore clinical outcome data and biomarkers to better understand NEPC.
This retrospective multicenter review was performed on 135 patients with high grade prostate cancer and morphological and/or immunohistochemical (IHC) features associated with NEPC. Among clinicopathological data collected for analyses were clinical stage, Gleason score, and serum biomarkers. The Kaplan-Meier method was used to describe overall survival (OS) and log-rank tests calculated for comparison. Cox proportional hazard regressions were employed to assess for prognostic impact of biomarkers at diagnosis, and as comparing between de novo NEPC and treatment-associated NEPC. Adjustments were made for clinical stage and presence of castration resistance.
As mentioned, 135 cases were identified, a majority of which were considered mixed tumors (92%, 124). Most cases were treatment-associated NEPC (59%) as compared de novo NEPC to (41%. In keeping with anticipation, 77% of cases with a Gleason score were grade group 5. Median PSA was 11.6 ng/mL prior to the biopsy diagnostic of NEPC. In contrast to other series, the disease states were quite variable at the time of NEPC diagnosis. 19 (14%) had localized disease, 33 (24%) non-metastatic castration sensitive disease, 35 (26%) metastatic castrate-sensitive disease, 6 (4%) non-metastatic castration resistant disease, and 42 (31%) metastatic castration resistant disease.
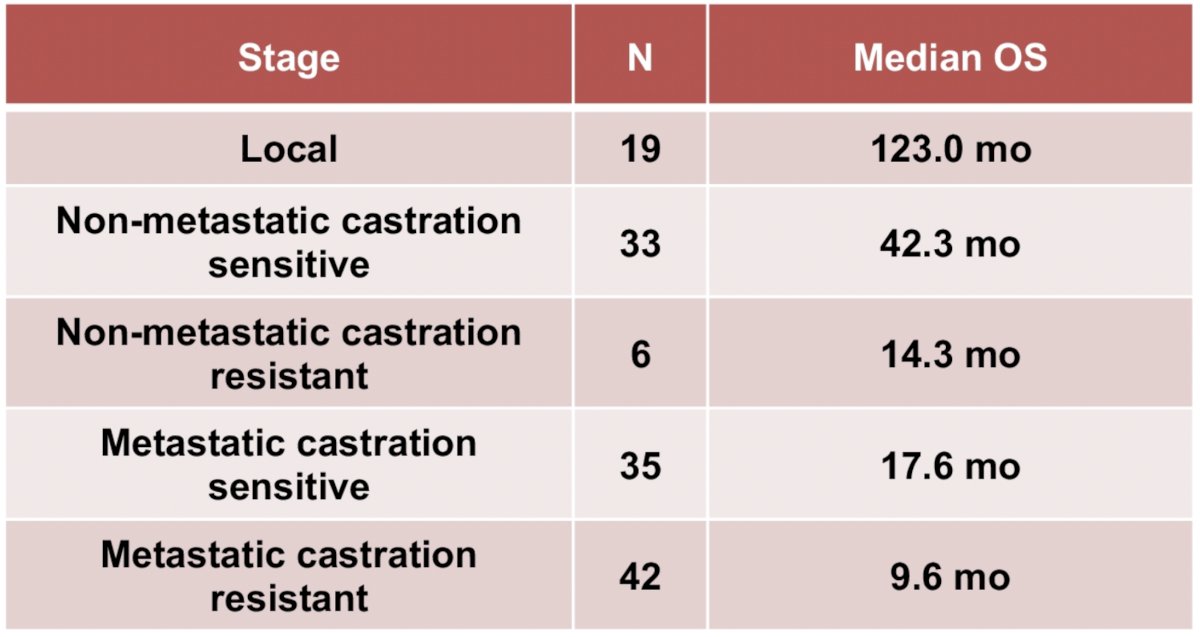
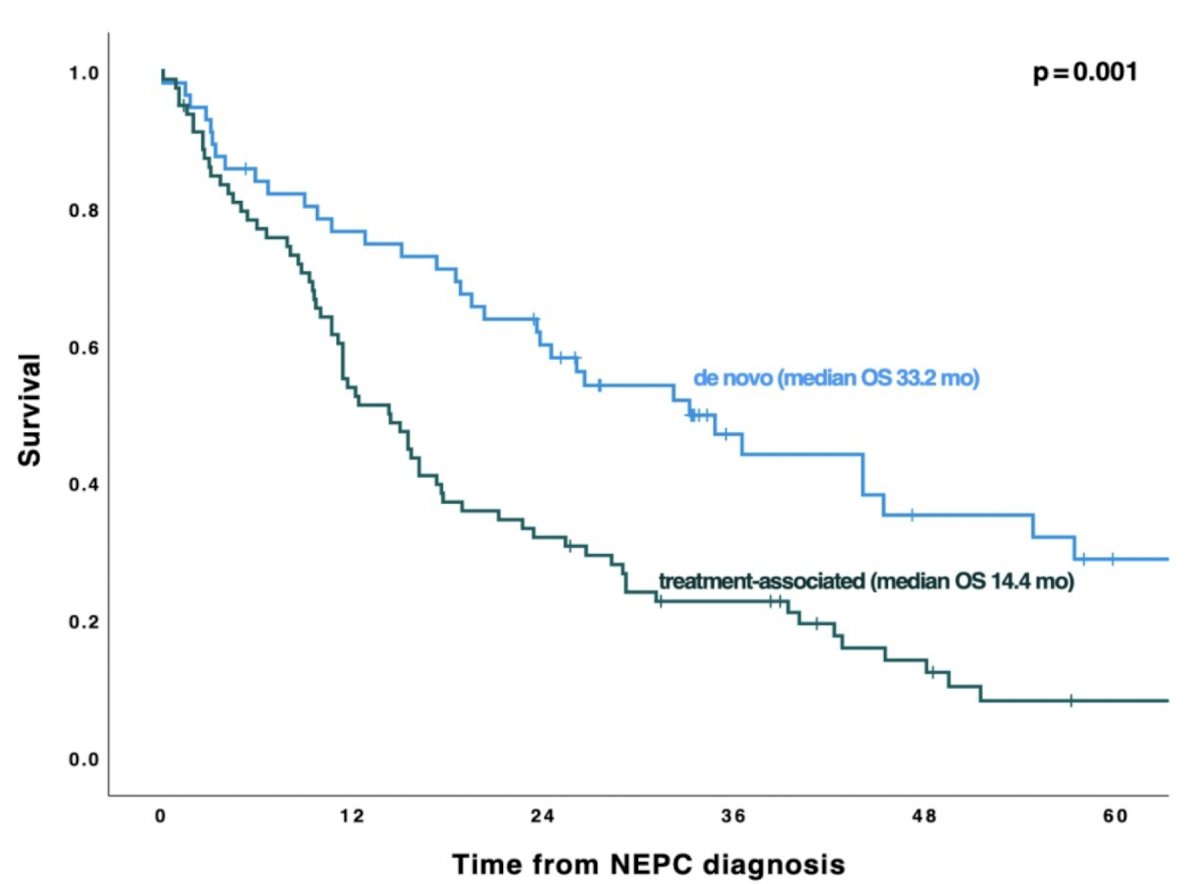
Median overall survival was longest in the localized tumors (123.0 months). Castration sensitive disease displayed OS of 42.3 when non-metastatic and 17.6 months when metastases were present. As expected, median overall survival was shorter in castration-resistant disease (nmCRPC: 14.3 months and mCRPC: 9.6 months). The authors also describe a significantly shorter median OS in those patient with treatment-associated NEPC (14.4 months) as compared to de novo NEPC (33.2 months, p =0.001).
Clinical variables including presence/absence and site of metastasis (visceral v non-visceral) were analyzed with shortest OS among those patients with visceral metastases (8.6 months, 95% CI 6.0-14.6) versus those with non-visceral (11.1 months, 95% CI 13.7-21.5) and an absence of metastases (42.3 months, 95% CI 47-89). Anemia and neutrophil-to-lymphocyte ratio >3 were both associated with modest increases in death (adjusted HR 1.66; 95% CI 1.05 - 2.16, p = 0.031; adjusted HR 1.51; 95% CI 1.01 - 2.52, p = 0.045). PSA level, Gleason score, and elevated serum LDH were not associated with differences in OS.
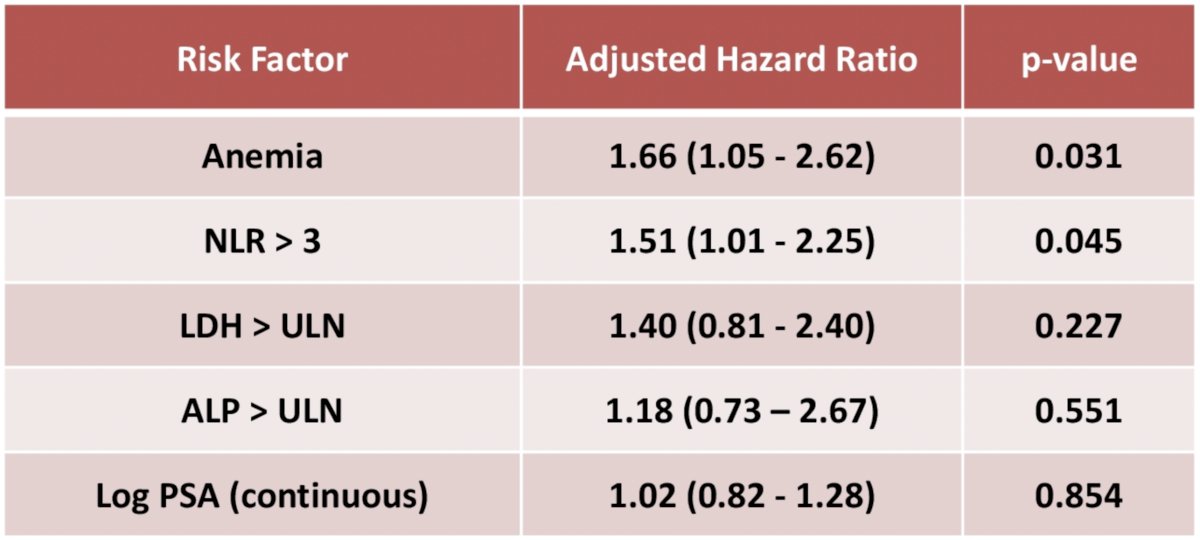
In conclusions, Gagnon et al. report on a robust dataset of NEPC and concluding that clinicopathological variables are associated with outcome. As expected, shorter OS was observed in patients with NEPC as compared to pure adenocarcinoma. The authors suggest that anemia and a neutrophil-to-leukocyte ratio of greater than 3 are prognostic and could be used to stratify patients for treatment intensification when available. Additional analyses are underway incorporating genomic data and IHC.
Presented by: Richard Gagnon, MD, BSc, University of Calgary
Written by: Jones Nauseef, MD, PhD, Assistant Professor of Medicine within the Division of Hematology and Medical Oncology, Sandra and Edward Meyer Cancer Center, and Englander Institute for Precision Medicine Weill Cornell Medicine and Assistant Attending physician at NewYork-Presbyterian Hospital. @DrJonesNauseef on Twitter during the 2023 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday Feb 16 – Saturday Feb 18, 20223


