(UroToday.com) The 2023 GU ASCO annual meeting included a session on advanced prostate cancer, specifically new targets, new drugs, and new victories, featuring a presentation by Dr. Gerhardt Attard discussing treatment combinations for patients starting androgen deprivation therapy (ADT). Dr. Attard started by highlighting the key sections of his talk (noting that in the context of the time allotted for his talk, it is impossible to cover all relevant trials):
- ADT + second generation ARSI
- Radiotherapy to the primary tumor
- Addition of docetaxel
ADT + Second Generation ARSI
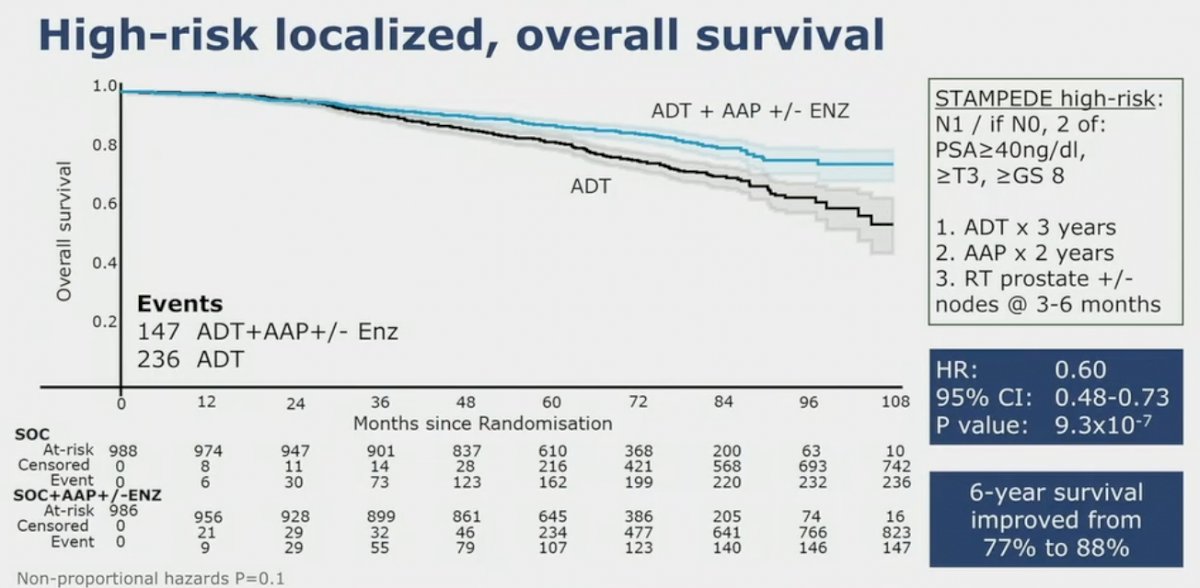
Dr. Attard notes that in the STAMPEDE arm of high-risk localized prostate cancer treated with either abiraterone or enzalutamide, there was a consistent effect with ARPI regardless of metastatic burden.1 In this study, local radiotherapy (as per local guidelines, 74 Gy in 37 fractions to the prostate and seminal vesicles or the equivalent using hypofractionated schedules) was mandated for node negative and encouraged for node positive disease. There were 1,974 patients randomized and over a median follow-up of 72 months (IQR 60–84), metastasis-free survival was significantly longer in the combination-therapy groups (median not reached, IQR NE–NE) than in the control groups (not reached, 97–NE; HR 0.53, 95% CI 0.44–0.64). The 6-year metastasis-free survival was 82% (95% CI 79–85) in the combination-therapy group and 69% (66–72) in the control group. Overall survival (median not reached [IQR NE–NE] in the combination-therapy groups vs not reached [103–NE] in the control groups; HR 0.60, 95% CI 0.48–0.73):
Dr. Attard notes that there are several outstanding questions in high-risk localized disease:
- “Lower risk” patients for ARSI? Better prognostication/risk stratification of localized cancers
- Can PSMA PET replace CT and bone scan to identify high-risk patients for ADT + abiraterone?
- Can the efficacy of ADT + abiraterone be extrapolated to ADT + AR antagonists?
- Will treatment effect be equivalent in men undergoing surgery?
- What is the ideal treatment duration?
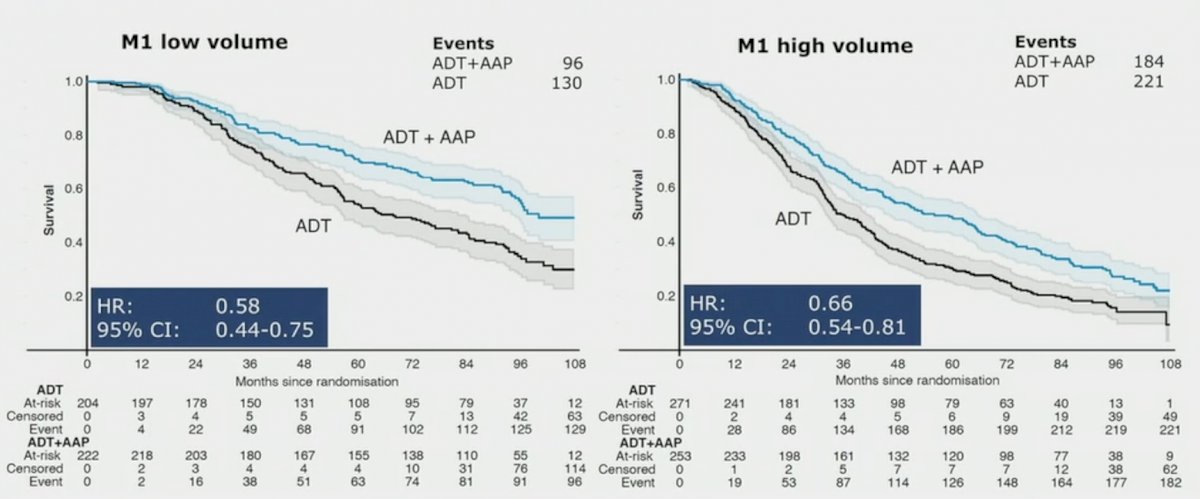
In a comparison of abiraterone acetate and prednisolone or combination enzalutamide + abiraterone acetate and prednisolone for mHSPC starting ADT presented at ESMO 2022, Dr. Attard noted that between November 2011 and January 2014, 1,003 patients were randomized to ADT +/- abiraterone acetate and prednisolone, and between July 2014 and March 2016, 916 patients were randomized to ADT +/- abiraterone acetate and prednisolone + enzalutamide. When looking at overall survival of M1 split by metastasis volume, there was a benefit for ADT + AAP for both M1 low volume and M1 high volume:
Dr. Attard notes that there should be consideration for de-intensification and for a finite duration, as highlighted by the following table:
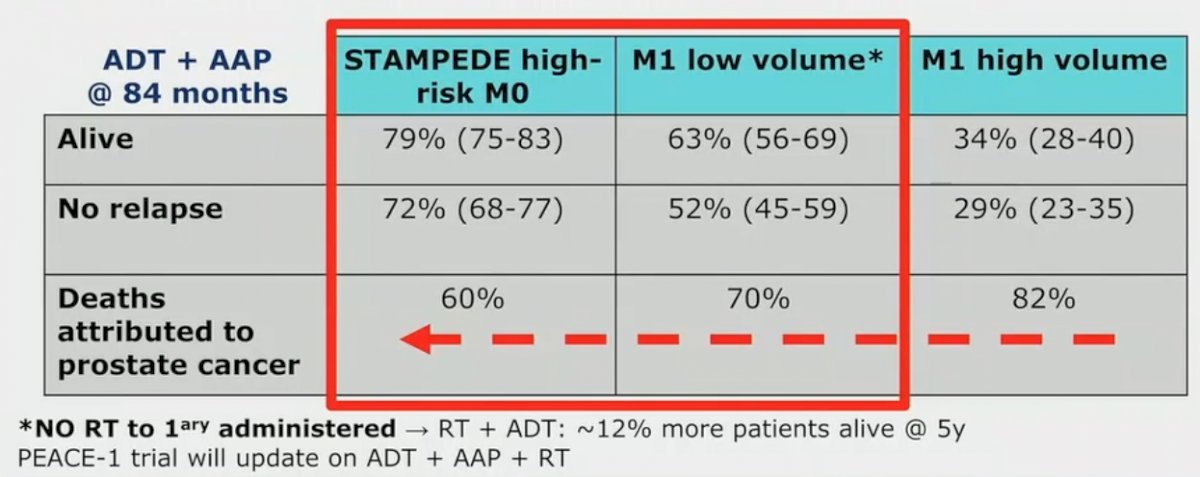
Dr. Tombal and Dr. Gillessen have suggested that for patients with low volume M1 disease, treatment should be de-intensified after a PSA reaches < 0.2 ng/mL after 6-12 months. Additionally, M1 phase III trials should be conducted only in selected poor prognosis groups or unnecessary harm will be caused to patients who are likely in remission >= 84 months.
Tests for stratification have used the STAMPEDE abiraterone, with data presented by Dr. Marina Parry at ESMO 2022 testing transcriptome signatures as prognostic and predictive biomarkers for patients starting ADT +/- abiraterone acetate and prednisolone. Of 1,917 patients (full trial cohort) enrolled from November 2011 - January 2014, 1,824 consented to tumor analysis. 1,298 (71%) were reviewed centrally, 831 (64%) gave transcriptomes, and 781 (94%) passed quality control. Of the 781, 50% vs 52% in full trial cohort were M1; other clinical variables, well balanced. The median follow-up was 94 months (IQR: 84 - 97). Neither AR-A, PAM50, PSC or the DECIPHER genomic classifier were predictive of treatment effect of abiraterone acetate + prednisolone on OS in the combined cohort (M0 and M1). However, the genomic classifier was strongly prognostic in advanced prostate cancer (per 0.1 increment, M1 OS (HR 1.18, 95% CI 1.09 - 1.26, p < 0.001), M0 MFS (HR 1.20, 95% CI 1.09 - 1.31, p < 0.001):
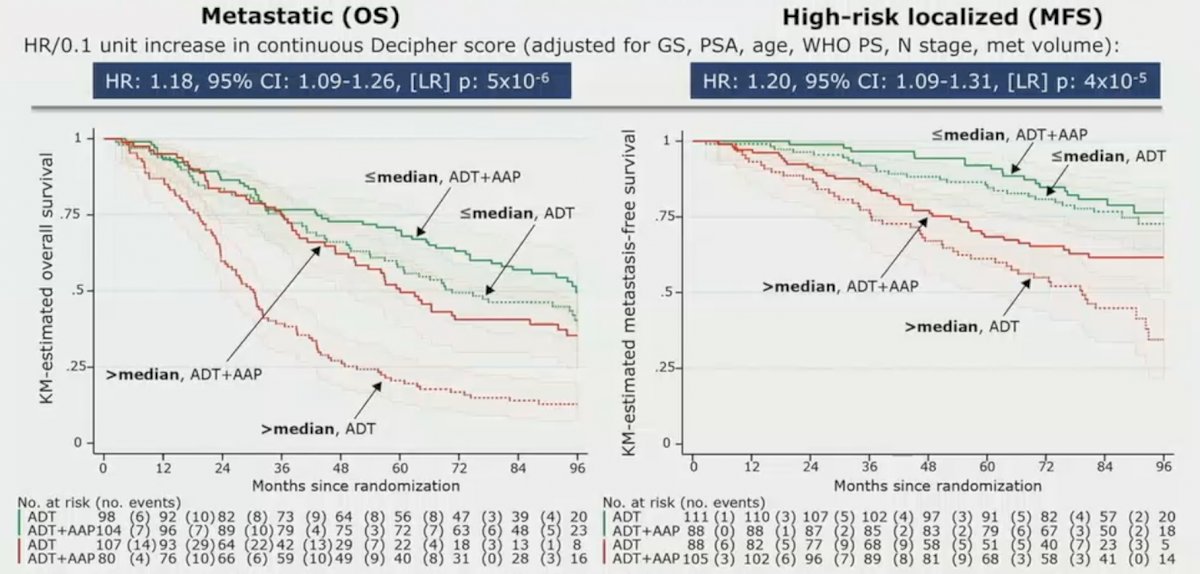
This study showed that the Decipher transcriptome signature can identify localized patients at increased risk of metastases/death at 84 months and consequently improve selection for ARSI.
Radiotherapy to the Primary Tumor
STAMPEDE (Arm H) was an open label, randomized controlled phase III trial of 2,061 men at 117 hospitals across Switzerland and the UK.2 This arm randomized patients with de novo mHSPC in a 1:1 fashion to standard of care + radiotherapy or standard of care alone between January 2013 and September 2016. Standard of care was defined as lifelong ADT with upfront docetaxel permitted from December 2015 onwards. Men allocated to radiotherapy received either a daily (55 Gy in 20 fractions over 4 weeks) or weekly (36 Gy in six fractions over 6 weeks) schedule that was nominated before randomization. The primary outcome for this trial was OS. Subgroup analysis by metastatic volume (CHAARTED criteria) was planned a priori. Median follow up for STAMPEDE Arm H was 37 months, median patient age was 68.0 years, and median PSA was 97 ng/ml. There were 18% of patients that received early docetaxel. In the overall cohort, RT improved failure-free survival (HR 0.76, 95% CI 0.68 to 0.84) but not overall survival (HR 0.92, 95% CI 0.80 to 1.06) in the overall cohort. However, when stratified by metastatic burden, OS benefits were seen in the low volume group (HR 0.68, 95% CI 0.52 to 0.90) with restricted mean survival time improved by 3.6 months from 45.4 to 49.1.
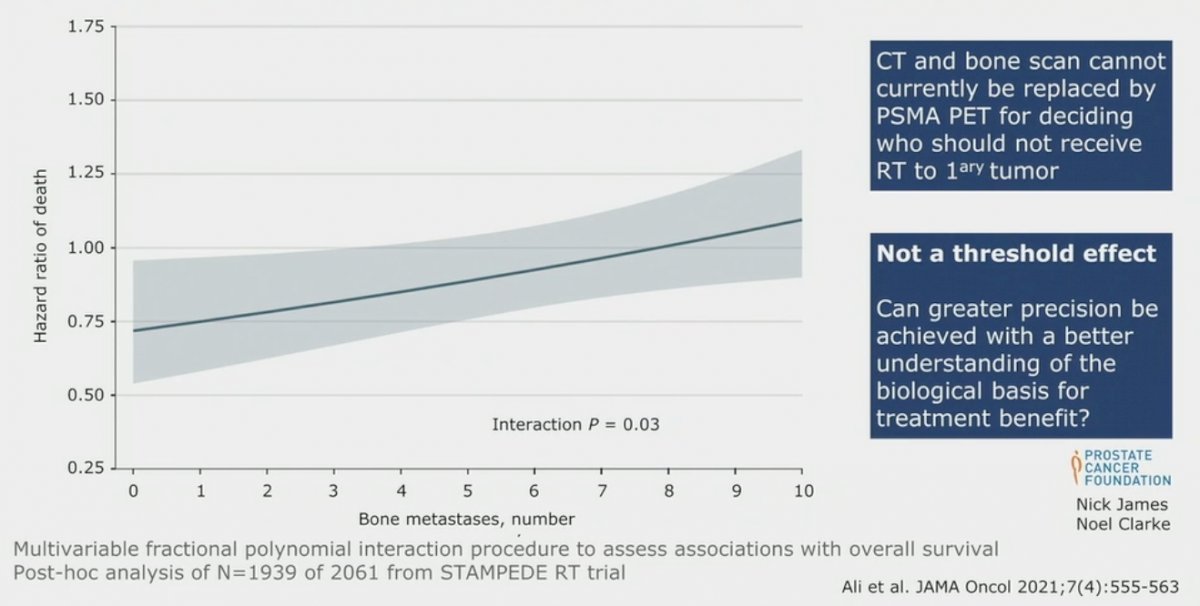
A secondary analysis of the STAMPEDE Arm H trial evaluating the association of metastatic burden with survival benefit from prostate radiotherapy demonstrated that the survival benefit decreased continuously as the number of bone metastases increased, with benefit most pronounced up to 3 bone metastases.3 The magnitude of benefit from the addition of prostate radiotherapy was greater in patients with low metastatic burden with only nonregional lymph nodes (M1a) or 3 or fewer bone metastases without visceral metastasis (HR for overall survival: 0.62; 95% CI: 0.46 - 0.83; HR for failure-free survival: 0.57; 95% CI: 0.47 - 0.70) than among patients with 4 or more bone metastases or any visceral/other metastasis (HR for overall survival: 1.08; 95% CI: 0.91 - 1.28; interaction p= 0.003; HR for failure-free survival: 0.87; 95% CI: 0.76 - 0.99; interaction p=0.002).
Addition of Docetaxel
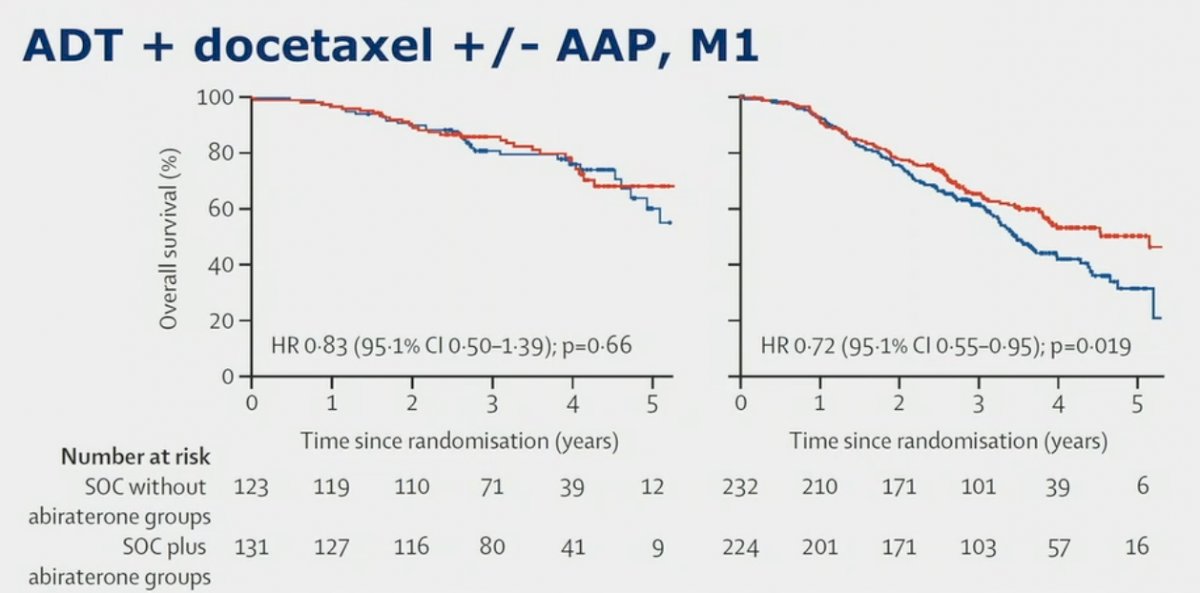
Dr. Attard notes that in the PEACE-1 trial,4 adding abiraterone to ADT + docetaxel improves survival, especially in high volume:
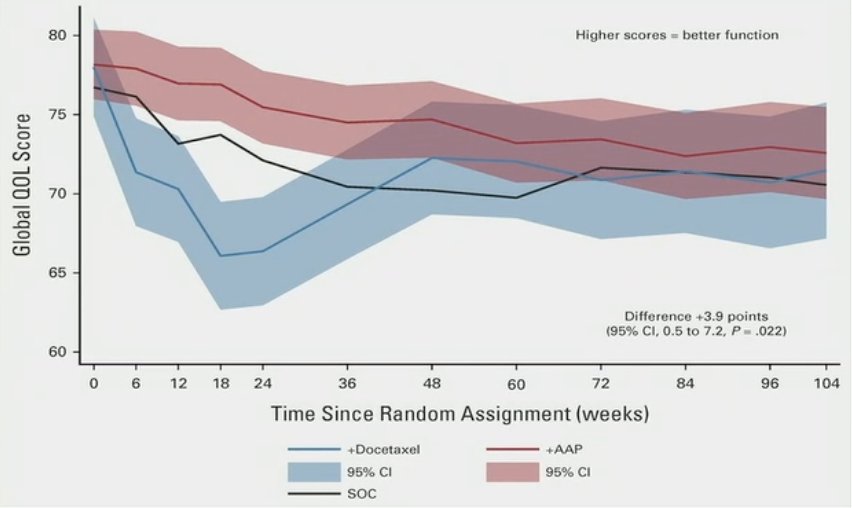
but what is the impact of adding docetaxel to ADT + abiraterone/other ARSIs? Additionally, we know there are implications for receipt of docetaxel, as patients receiving standard of care + abiraterone acetate + prednisone reported clinically meaningful higher global-QOL scores through the first year.5 Furthermore, quality of life scores were superior over 2 years but narrowly missed the predefined value for clinical significance
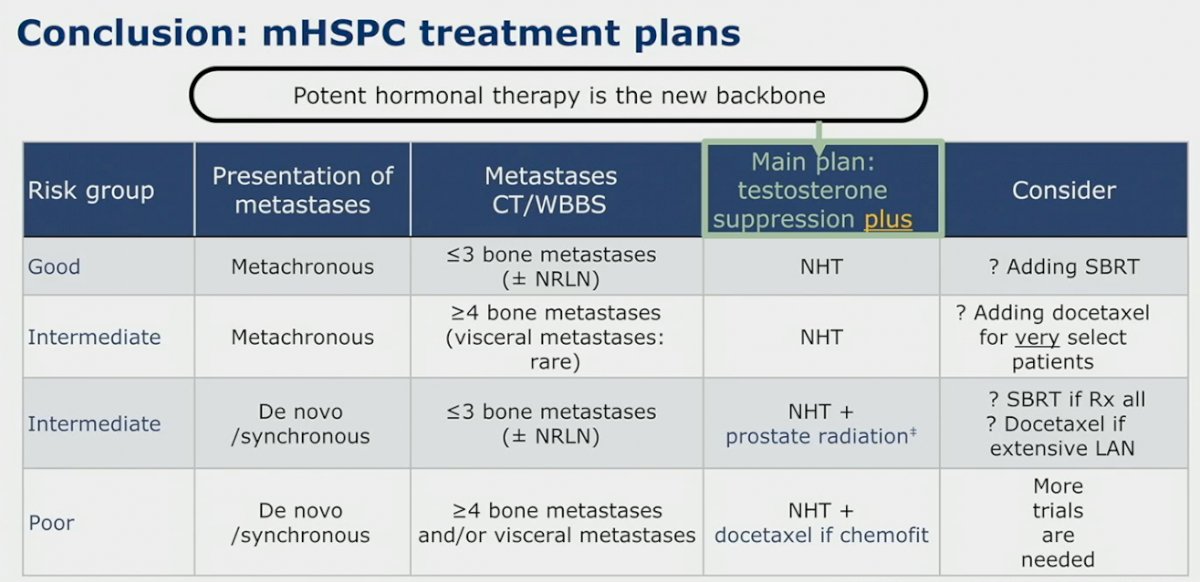
Dr. Attard concluded his presentation discussing treatment combinations for patients starting ADT by highlighting mHSPC treatment plans provided by Dr. Chris Sweeney at the 2022 APCCC meeting:
Presented by: Gerhardt Attard, University College London Cancer Institute, London, UK
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 Genitourinary (GU) American Society of Clinical Oncology (ASCO) Annual Meeting, San Francisco, Thurs, Feb 16 – Sat, Feb 18, 2023.
References:
- Attard G, Murphy L, Clarke NW, et al. Abiraterone acetate and prednisolone with or without enzalutamide for high-risk non-metastatic prostate cancer: A meta-analysis of primary results from two randomized controlled phase 3 trials of the STAMPEDE platform protocol. Lancet 2022 Jan 29;399(10323):447-460.
- Parker CC, James ND, Brawley CD, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): A randomized controlled phase 3 trial. Lancet 2018 Dec 1;392(10162):2353-2366.
- Ali A, Hoyle A, Haran AM, et al. Association of Bone Metastatic Burden with Survival Benefit from Prostate Radiotherapy in Patients with Newly Diagnosed Metastatic Prostate Cancer: A Secondary Analysis of a Randomized Clinical Trial. JAMA Onc 2021 Apr 1;7(4):555-563.
- Fizazi K, Foulon S, Carles J, Roubaud G, et al. Abiraterone plus prednisone added to androgen deprivation therapy and docetaxel in de novo metastatic castration-sensitive prostate cancer (PEACE-1): A multicentre, open-label, randomized, phase 3 study with a 2 x 2 factorial design. Lancet. 2022 Apr 30;399(10336):1695-1707.
- Rush HL, Murphy L, Morgans AK, et al. Quality of Life in Men with Prostate Cancer Randomly Allocated to Receive Docetaxel or Abiraterone in the STAMPEDE trial. J Clin Oncol. 2021;40:825-836.


