(Urotoday.com) On the first day of the American Society for Clinical Oncology (ASCO) Genitourinary Cancer Symposium 2023 focussing on prostate cancer, Dr. Geoffrey Gotto presented administrative data from Alberta, Canada in Poster Session A, examining the practice patterns of treatment intensification in patients with metastatic castration-sensitive prostate cancer.
Over the past few years, treatment intensification employing either docetaxel or a novel hormonal therapy in addition to androgen deprivation therapy (ADT) has become standard of care for patients with metastatic castration-sensitive prostate cancer (mCSPC), based on consistently demonstrated survival benefits. However, real world data have demonstrated somewhat poor uptake of these approaches with significant variation between jurisdictions.
To better understand uptake of these approaches, the authors used electronic medical records and administrative data to perform a population-based retrospective cohort study among patients aged ≥18 years of age who were newly diagnosed with de novo mCSPC and initiated ADT post-diagnosis between 2010 to 2020 in Alberta, Canada. Treatment intensification was defined as the receipt of apalutamide, abiraterone acetate, enzalutamide, or chemotherapy (e.g. docetaxel) within 180 days of ADT initiation.
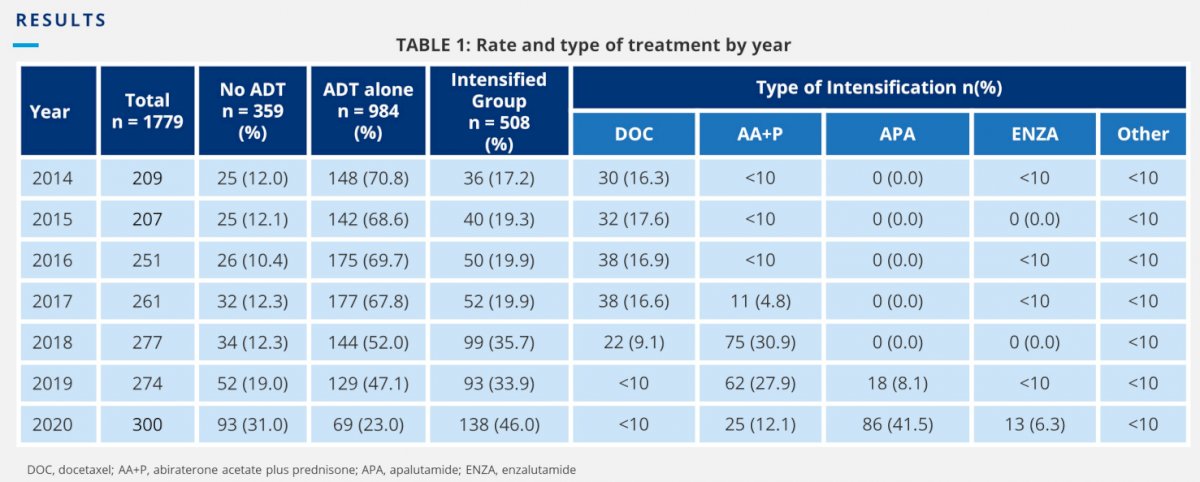
The authors identified 2,515 patients with de novo mCSPC during study period of whom 2,098 (83%) initiated ADT post-diagnosis. Of those 2098 patients, 525 (25%) received intensification beyond ADT. The percentage of patients who were intensified was 3% in 2010-2013 and gradually increased to 67% in 2020. Between 2014-2017, docetaxel was the most common therapy for intensification, but its use decreased considerably in 2018-2020 with abiraterone acetate, apalutamide and enzalutamide becoming increasingly available in the mCSPC setting.
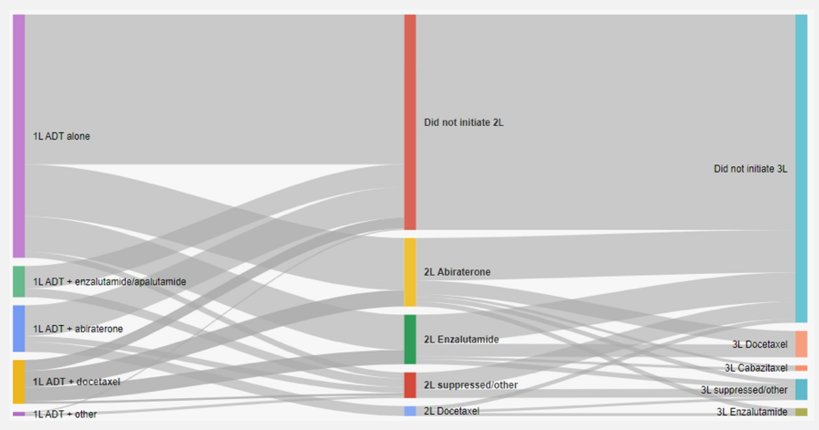
Upon progression (ie. to mCRPC), 46% and 22% in the intensified group versus 38% and 13% in the ADT-alone group initiated one and two-lines of subsequent therapies respectively. Abiraterone acetate and enzalutamide were the most common subsequent therapy for both the intensified (32% and 31% respectively) and the ADT-alone (56% and 38% respectively) groups. Docetaxel (24%) was used as subsequent therapy among mCSPC patients who were intensified with oral systemic agents.
In multivariable logistic regression analyses of patients diagnosed in 2014-2020 (a time period in which treatment intensification use increased substantially), significant predictors of intensification were younger age at diagnosis, lower Charlson comorbidity index, greater number of metastatic sites, shorter time to ADT initiation, referral to a specialists/cancer centres, surgery or radiation prior to ADT, and more recent year of diagnosis (all p<0.05).
Thus, the authors demonstrate that in Alberta, Canada, there has been a considerable increase in the utilization of ADT intensification therapies that correspond with the timing of clinical trial data and approvals of novel agents. Early referral to specialists/cancer centres is warranted to intensify mCSPC treatment beyond ADT and to improve patients’ outcomes.
Presented by: Geoffrey T. Gotto, MD, MPH | Southern Alberta Institute of Urology, University of Calgary

