(UroToday.com) The first day of the American Society for Clinical Oncology (ASCO) Genitourinary Cancer Symposium 2023 began with four talks highlighting key data that, from the perspective of medical oncologists, urologic oncologists, radiation oncologists, and pathologists, advanced the needle in prostate cancer care in 2023.
Third among these talks is one from Dr. Angela Jia, presenting from the point of view of a radiation oncologist. By way of introduction and overview, she emphasized that there have been important advances in understanding treatment approaches for patients with both newly diagnosed and recurrent disease, including considerations regarding radiotherapy fractionation, the use of concurrent androgen deprivation therapy, and biomarkers for prognostication.
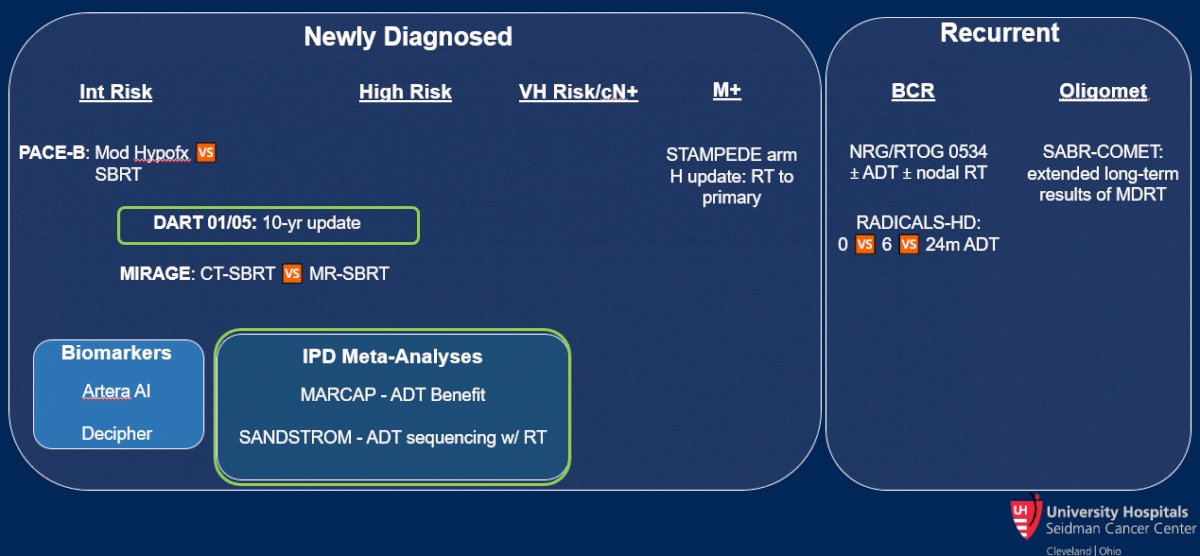
She first discussed the long-term results of the DART 01/05 trial, a randomized comparison of definitive radiotherapy with either short or long-duration of androgen deprivation therapy (ADT) in patients with intermediate and high-risk disease. While there was no significant benefit in overall survival in the intention to treat population, Dr. Jia noted that there is a suggested benefit among those with higher risk disease.

Taking a wider view of the question of concomitant ADT in patients undergoing definitive radiotherapy, she then highlighted results from the MARCAP consortium who published an individual patient-data meta-analysis assessing this question. Regardless of radiotherapy dose, patients receiving radiotherapy had improved biochemical recurrence rates, distant metastasis rates, metastasis-free survival, and overall survival when treated with ADT.
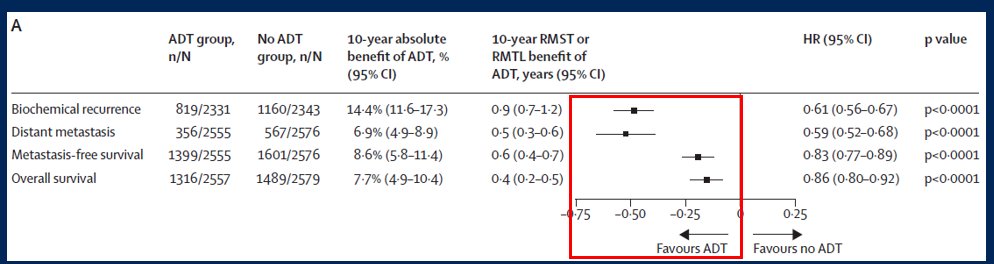
When considering the number needed to treat for 10-year distant metastasis, among the intermediate risk group this is 18.0 while it falls to 8.4 men with high-risk disease.
Beyond the question of whether to give ADT, the MARCAP consortium further assessed the question of ADT prolongation, comparing short-term to long-term ADT. Adjuvant ADT for 18 months or longer was associated with improved metastasis-free survival (HR 0.84, 95% CI 0.78-0.91) and overall survival (HR 0.85, 95% CI 0.78-0.94). Correspondingly, the number needed to treat to prevent one event for 10-year distant metastasis was 16.1 for men with intermediate risk disease and 10.4 for those with high-risk disease. However, neoadjuvant prolongation (ie. giving ADT for a longer period prior to starting radiotherapy) was not associated with improvements in either metastasis-free or overall survival.
Dr. Jia then discussed results of the SANDSTORM analysis which assessed the question of the timing of short-duration ADT for patients undergoing radiotherapy for non-metastatic prostate cancer based on a pooled analysis of 12 randomized trials. Again relying on individual patient-data meta-analysis, the authors found improved outcomes for patients receiving concurrent and adjuvant ADT, as compared to neoadjuvant and concurrent ADT, along with prostate-only radiotherapy.

Dr. Jia then moved to discussing new data in biomarkers for patients with prostate cancer. She noted that the Decipher assay is both prognostic for the development of distant metastatic disease (with those patients having high Decipher risk harbouring a 4-fold risk of metastasis at 10-years compared to those with low Decipher risk, 16% vs 4%) and also predictive of the benefit of radiotherapy dose escalation. In a secondary analysis of the RTOG 0126 phase III trial of dose escalation in patients with intermediate risk prostate cancer, those with low Decipher GC risk derived a relatively smaller benefit (5%) from dose escalation while those with intermediate or high Decipher GC risk derived a relatively large benefit (26% decreased risk of metastasis).

However, there are ongoing efforts to improve prognostication and risk stratification. One important approach that has made substantial leaps over the past year is the development and validation of a multi-modal artificial intelligence (MMAI) predictive biomarker. This was developed using the NRG Biobank based on approximately 4,000 patients included in a number of RTOG trials. Using the patient demographics, clinical data, and digital pathology imagery, a predictive tool was developed to predict distant metastasis. This was subsequently validated among patients enrolled on the NRG/RTOG 9408 trial to provide an ability to assess the biomarker-treatment interaction and assess the predictive ability for ADT intensification.

In doing so, Dr. Jia highlighted that MMAI predicted the benefit (in terms of distant metastasis) from the addition of ADT to radiotherapy: in patients who were biomarker negative, there was a negligible benefit to the addition of ADT; however, in those who were biomarker positive, the 15-year metastasis rates were decreased by nearly 10% (from 15.2% with RT alone to 5.4% with the addition of ADT; hazard ratio 0.33, 95% CI 0.19-0.57).

Dr. Jia then considered questions relating to the delivery of radiotherapy. First among these, she discussed the PACE-B trial, a phase III comparison of moderate hypofractionation with SBRT. Importantly, this non-inferiority trial included patients with low and intermediate risk disease who did not receive ADT. While the primary outcome is biochemical and clinical failure, data published in 2022 highlighted 2-year toxicity results. Dr. Jia noted that while there was a similar incidence of late grade 2 or greater genitourinary toxicity between the two groups, there appeared to be a higher burden of patient-reported bother among those who received SBRT.

In terms of gastrointestinal toxicity, there was a similar incidence of late grade 2 or greater toxicity that corresponded to patient reported outcomes.
The second key study examining radiotherapy treatment approaches that Dr. Jia highlighted was the MIRAGE trial, comparing MRI vs CT guided SBRT. Likely driven by the decreased margins allowable with the MRI approach, MRI-guided SBRT was associated with decreased rates of acute genitourinary and gastrointestinal toxicity. In terms of grade 2 genitourinary toxicity, this manifest as a 60% reduction in the odds on multivariable analysis.
Dr. Jia then highlighted data from Arm H of STAMPEDE assessing the role of radiotherapy to the prostate in patients with metastatic disease. As has been previously reported, this study included patients with de novo mHSPC who had not received prior radical treatment and who had disease as measured on conventional imaging. Patients were randomized to receive standard of care (ADT with or without docetaxel) with or without radiotherapy. In an updated analysis published in PLoS Medicine in 2022, Dr. Parker and colleagues demonstrated improved overall survival among those with a low metastatic burden (HR 0.64, 95% CI 0.52-0.79).

While the aforementioned studies focused on patients with newly diagnosed disease, Dr. Jia then described new data for patients with recurrent disease, highlighting first the SPPORT trial in patients with biochemical recurrent. This study evaluated the addition of both androgen deprivation therapy and pelvic lymph node radiotherapy for patients undergoing salvage prostate bed radiotherapy. Patients were randomized into three groups: Arm 1 received prostate bed radiotherapy alone, Arm 2 received prostate bed radiotherapy with short term (4-6 months) of ADT, and Arm 3 received prostate bed radiotherapy, short-term ADT, and pelvic nodal radiotherapy.
In terms of the comparison between arms 2 and 3, Dr. Jia noted that the addition of nodal radiotherapy provides a small, but significant, failure-free progression benefit.
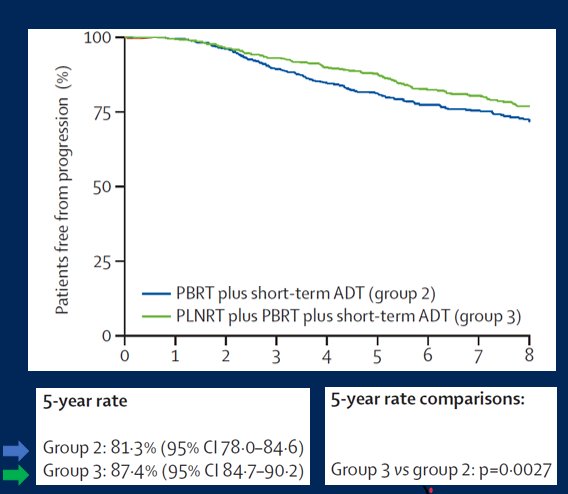
However, this effect was larger among patients with a higher PSA (greater than the median, 0.35ng/mL) at the time of salvage radiotherapy.
Putting this study in context of other trials (RTOG 9601 and GETUG-16), Dr. Jia noted that there is no clear benefit to adding hormone therapy to early salvage radiotherapy.
Continuing further with the question of the role of ADT for patients undergoing salvage therapy for biochemically recurrent disease, Dr. Jia then discussed the RADICAL-HR publication. This randomized comparison showed improved metastasis-free survival for patients undergoing 24 months of ADT (compared to none) but not 6 months of ADT (compared to none). Further, the comparison between short and long durations of ADT showed a significant improvement in 10-year metastasis-free survival (72 vs 78%; HR 0.77, 95% CI 0.61-0.97) with a corresponding number needed to treat of 17.
These data were then aggregated in the DADSPORT meta-analysis which demonstrated no overall survival benefit to the addition of ADT to salvage radiotherapy.

Finally, Dr. Jia considered recent data regarding the role of radiotherapy in oligometastatic disease. Updated data from the SABR-COMET trial showed that this increased duration of follow-up resulted in a larger absolute benefit of the addition of metastasis-directed therapy, without any new safety signals.
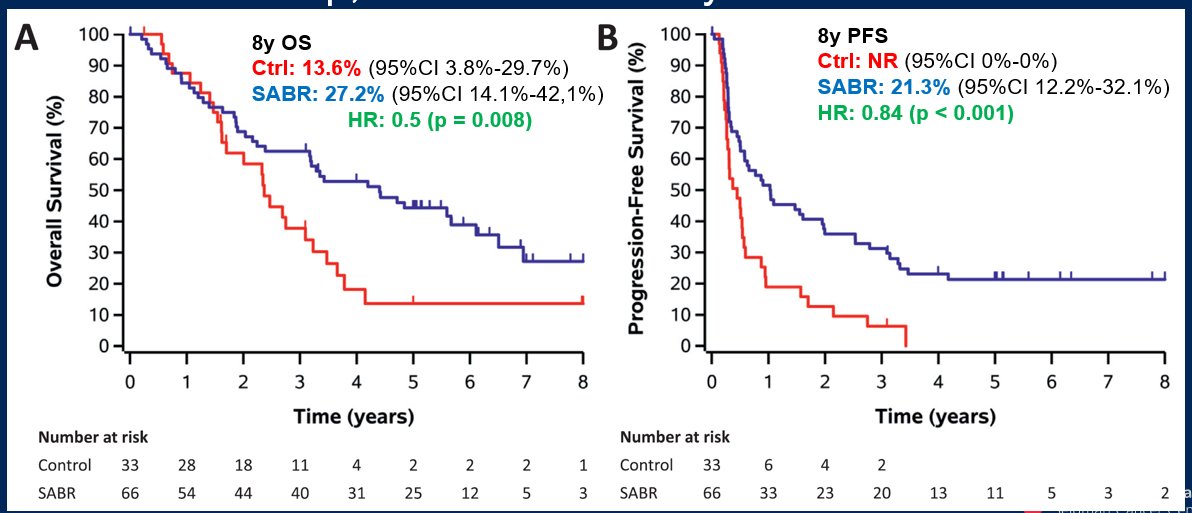
Thus, Dr. Jia concluded by noting that, for patients with newly diagnosed disease, for patients with intermediate risk disease, there is a benefit to short-term ADT, regardless of RT dose. Further, adjuvant ADT is superior to neoadjuvant ADT. Moving forward Decipher can prognostically identify patients at lower risk of recurrence whereas ArteraAI is currently prognostic and soon to be predictive of the benefit of ADT in intermediate risk disease. For those with high-risk disease, she noted that long-term ADT is beneficial regardless of RT dose. Further, in patients with low-volume metastatic disease, there is an overall survival benefit to the use of prostate radiotherapy, though we must work on how we apply these data to patients staged with PSMA-PET/CT. Further, she noted that SBRT has become a standard of care in the US: as a result, the PACE-B results are reassuring while MIRAGE suggests that adoption of MRI-guidance may further improve the toxicity profile.
Among those with recurrent or oligometastatic disease, Dr. Jia highlighted that the role of ADT with salvage radiotherapy remains complex. There is an unmet need for biomarker guidance to identify those who will benefit. She additionally noted that there are a number of forthcoming studies at this meeting that will provide further data to guide this disease space. Follow the UroToday coverage of the meeting for these data.



