TRISST is a phase III, multicenter, non-inferiority, factorial trial. Eligible men had undergone orchiectomy for stage I seminoma with no adjuvant therapy planned. Randomization was to:
- 7 CTs: 6, 12, 18, 24, 36, 48, 60 months after randomization
- 7 MRIs: 6, 12, 18, 24, 36, 48, 60 months after randomization
- 3 CTs: 6, 18, 36 months after randomization
- 3 MRIs: 6, 18, 36 months after randomization
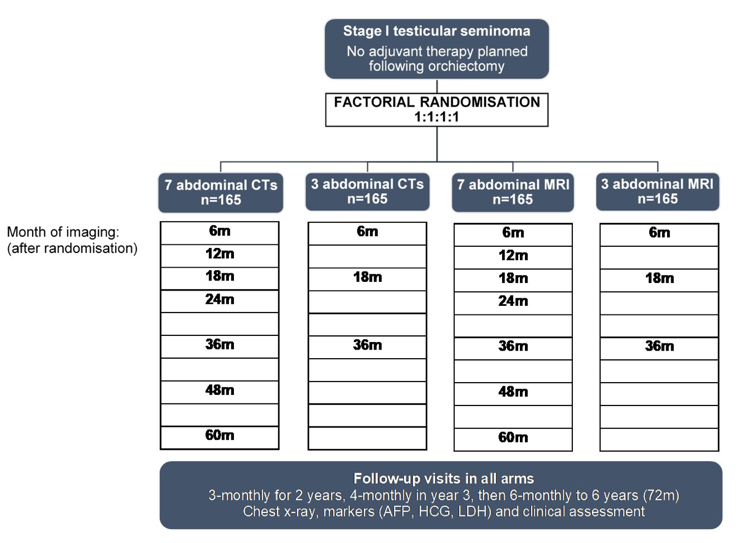
Follow-up for the trial was for 6 years with a primary outcome of 6-year incidence of stage ≥IIC relapse, aiming to exclude an increase ≥5.7% (from 5.7% to 11.4%) with MRI (versus CT) or 3 scans (versus 7). The target sample size was 660 patients, all contributing to both comparisons. Secondary outcomes include relapse ≥3cm, disease-free and overall survival.
There were 669 men enrolled from 35 UK centers (2008-2014), with a mean tumor size of 2.9 cm, and 358 (54%) were low risk (≤4cm, no rete testis invasion). In those patients remaining on surveillance, compliance was good with 94% of scans attended, 79% on time (+/- 4 weeks). Median follow-up was 72 months over which 82 (12%) patients relapsed. Incidence of stage ≥IIC relapse was low in all groups (n=10). More events occurred with 3 scans compared to 7 scans, though non-inferior based on design criteria: 9 (2.8%) versus 1 (0.3%), 2.5% increase (90% CI 1.0% to 4.1%; intent-to-treat). In the 3-scan arms 4/9 relapses could potentially have been detected earlier with the 7-scan schedule:
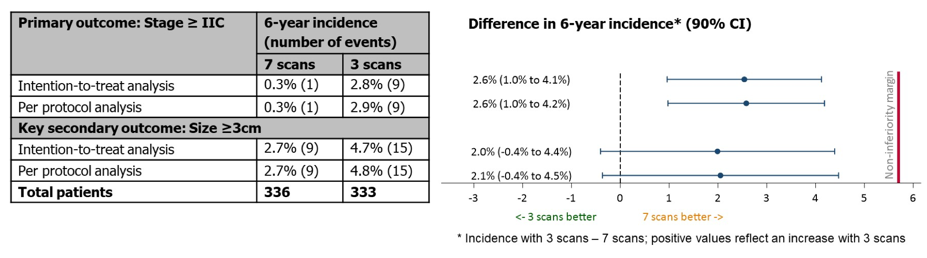
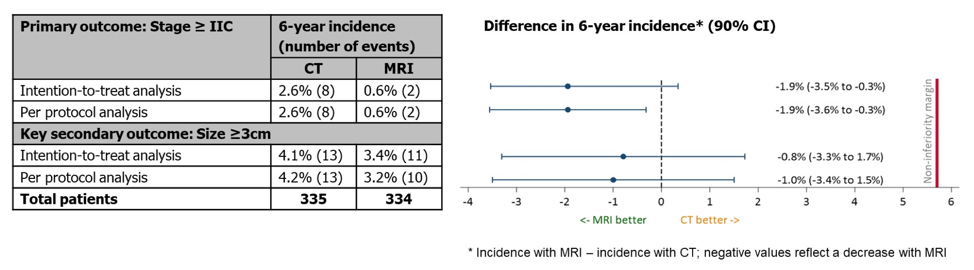
Fewer events occurred with MRI versus CT: 2 (0.6%) versus 8 (2.5%), 1.9% decrease (90% CI -3.5% to -0.3%; intent-to-treat). Incidence of relapse ≥3cm was 3.7% and non-inferiority was shown for both comparisons:
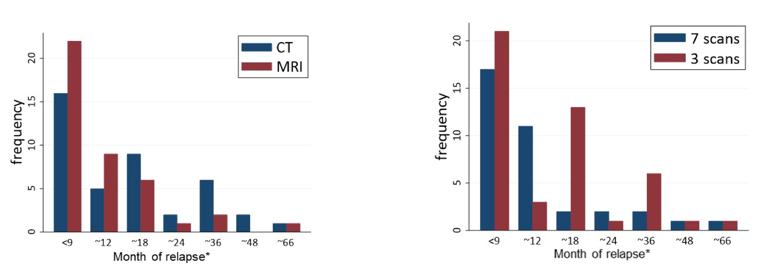
In all groups, most relapses were detected at scheduled imaging, very few occurred beyond 3 years (5 in 558 at risk, <1%):
Relapse treatment outcomes were good (81% complete response) with no tumor-related deaths. Treatment for stage >=IIC was typically BEP x3 or BEP x4, although 16/72 (22%) of patients with lower stage also received BEP. 5-year disease-free survival was 87% and for overall survival 99% and similar across groups.
Dr. Huddart concluded his presentation of TRISST with the following take-home points:
- Incidence of advanced relapse was very low regardless of imaging modality or frequency
- Treatment for relapse was successful and long-term outcomes were excellent in all arms, with no deaths due to testicular cancer
- MRI is non-inferior to CT, avoids irradiation, and should be recommended
- A 3-scan schedule was non-inferior to 7 scans
- Relapses beyond 3 years was rare
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_mdduring the 2021 American Society of Clinical Oncology Genitourinary Cancers Symposium (#GU21), February 11th-February 13th, 2021


