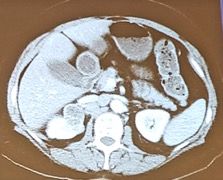
Dr. Choueiri started by discussing appropriate work-up, specifically imaging. Dr. Meng, a urologist, would get a CT of the chest, but probably would not do a bone-scan. Dr. Kollmannsberger, a medical oncologist, notes that there is no clear role regarding the utility of PET-CT imaging and rather relies on conventional imaging. Dr. Choueiri then discussed biopsy vs surgical removal – Dr. Meng states that he would proceed with biopsy to further delineate if he would operate (favor biopsy of the kidney). Dr. Clark, a urologist, poses the question that if the remaining staging imaging were negative, would it be appropriate to proceed directly to surgery without biopsy? Dr. Kollmannsberger completely agrees, that there is not necessarily a role for biopsy here if imaging is otherwise unremarkable and he would favor a nephrectomy and lymphadenectomy. Dr. Gore, a urologjst, notes that it is appropriate to perform a lymphadenectomy for radiographically evident lymphadenopathy, but there is no evidence for routine lymphadenectomy with radiographically negative lymph nodes.
Dr. Choueiri notes that this patient did end up having a biopsy of the kidney, which demonstrated papillary architecture with a fibrovascular core lined by a pseudostratified layer of cells. Given this situation, Dr. Choueiri then reposes options for this patient. Dr. Gore notes that there are unlikely to be non-surgical options as he feels that this is likely a papillary type II histology. Dr. Albiges, a medical oncologist, also agrees that the next step would be a radical nephrectomy (which they did). The pathologic staging of the tumor was T3aN1 stage III papillary RCC, intermediate grade.
Dr. Choueiri posed the question regarding a potential role for adjuvant therapy in this patient to which Dr. Albiges notes that most open trials are immunotherapy adjuvant trials, but not all are enrolling non-ccRCC patients. Dr. Kollmannsberger would not extrapolate S-TRAC data (only ccRCC histology) to a non-ccRCC patient regarding adjuvant sunitinib. Dr. Choueiri then highlighted the following excellent summary slide of the current immunotherapy trials ongoing in the perioperative setting:

Dr. Choueiri asked the question “considering that immunotherapy is better tolerated than TKIs, if these adjuvant immunotherapy studies have a PFS but no OS advantage, would you treat?” Dr. Kollmannsberger notes that he may treat, but it depends on the magnitude of the benefit, as well as the patient’s desires. Dr. Albiges agrees and reiterates the importance of the toxicity profile.
Dr. Choueiri then highlighted that this patient’s chest CT scan was positive for five pulmonary nodules, however no other sites of metastases. Dr. Choueiri then asked Dr. Meng about the utility of cytoreductive nephrectomy for this patient and whether he would consider metastasectomy for the lung lesions. Dr. Meng notes that the primary mass is small and given the number and volume of lung metastases he would not necessarily immediately proceed to cytoreductive nephrectomy. However, the caveat is that this is non-ccRCC and the decision regarding cytoreductive nephrectomy is not clear-cut. Dr. Atwell, an interventional radiologist, notes that it would be challenging to do SBRT for this many pulmonary lesions, however he thinks it is feasible to perform ablation for up to 3-4 lung lesions. Outside of a clinical trial, Dr. Albiges would opt for a VEGF inhibitor for which most of the data favors sunitinib (to which Dr. Kollmannsberger agrees). However, Dr. Kollmannsberger does note that given the location and volume of metastases, he would consider systemic therapy up front prior to local treatment of the kidney and/or lung lesions. Dr. Kollmannsberger also notes that cabozantinib may be an option for this patient in the first-line.
Chairs:
Peter E. Clark, Levine Cancer Institute, Atrium Health, Charlotte, NC
Toni K. Choueiri, Dana-Farber Cancer Institute, Boston, MA
Panelists: Christian K. Kollmannsberger, BC Cancer – Vancouver Prostate Centre, Vancouver, BC, Canada; John L. Gore, University of Washington, Seattle, WA; Maxwell V. Meng, UCSF, San Francisco, CA; Thomas D. Atwell, Mayo Clinic, Rochester, MN; Laurence Albiges, Institut Gustave Roussy, Universite Paris-Sud, Villejuif, France
Written By: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter:@zklaassen_md at the 2019 American Society of Clinical Oncology Genitourinary Cancers Symposium, (ASCO GU) #GU19, February 14-16, 2019 - San Francisco, CA


