The investigators utilized the IMDC (International mRCC Database Consortium) database that has data on ~9,000 patients with metastatic RCC. Patients were selected who had synchronous metastatic disease at the time of nephrectomy to assure that only cytoreduction was being studied. They identified 244 pRCC patients that met these criteria. These patients had documented IMDC risk criteria, which were subsequently controlled for in the multivariable analysis.
Patients who received CN tended to be younger (59yo vs. 67yo), but were otherwise relatively similar in terms of IMDC criteria and types of metastases. There were similar response rates to initial systemic therapy in both groups. After CN, there did appear to be a significant difference in both PFS and OS between those who received CN and those who did not. The Kaplan-Meier survival curves are shown below. The median PFS for CN was 5.1 months vs. 3.4 months (p=0.0344). The median overall survival for CN was 16.3mo vs. 8.6 mo (p<0.0001). The HR after adjusting for IMDC risk factors was 0.62 for those who received CN.
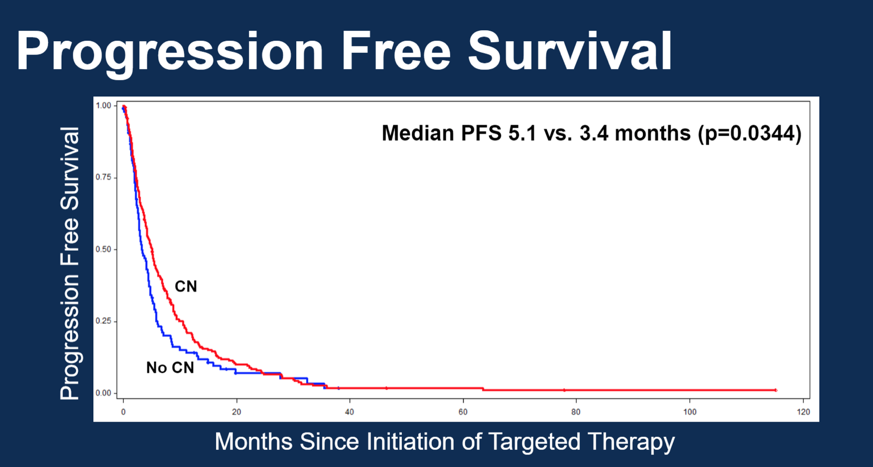
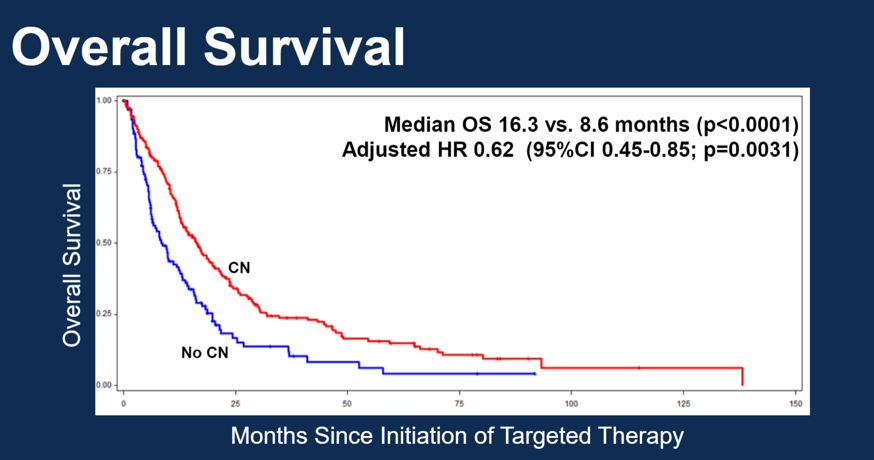
In conclusion, analysis of the IMDC database appears to reveal that patients with metastatic pRCC do benefit from CN, both in terms of PFS and OS. Likely due to some element of selection bias, younger patients were more likely to receive a CN. These findings appear to be in line with other large retrospective studies analyzing the use of CN in metastatic pRCC; and the consistent signal may be pointing to a real benefit for these patients to receive CN.
Of course, this study and others like it are limited by their retrospective nature and all of its inherent unmeasured biases. However, prospective trials with such rare cancers may not be possible, so further exploration of retrospective data and use of stratified prospective data may help validate these findings in the future. In real-world practice, most Urologists would offer CN to patients with metastatic pRCC who can tolerate surgery, so these results are reassuring that CN is still an appropriate practice.
Presented by: Jeffrey Graham, MD; Multi-institutional Collaborative
Written by: Shreyas Joshi, MD, Fox Chase Cancer Center, Philadelphia, PA at the 2018 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, February 8-10, 2018 - San Francisco, CA


