(UroToday.com) The 2023 American Society of Clinical Oncology (ASCO) annual meeting held in Chicago, IL between June 2nd and June 6th was host to a kidney and bladder cancers poster session. Dr. Audreylie Lemelin presented an analysis from the International mRCC Database Consortium (IMDC) characterizing subsequent treatment patterns in metastatic renal cell carcinoma (mRCC) patients progressing following nivolumab plus ipilimumab.
Dr. Lemelin began by noting that treatment patterns and number of lines of therapy for patients with mRCC are not well characterized in the era of immunotherapy-based combinations. In this study, the authors sought to quantify the attrition rates by line of therapy and to examine predictors of receiving 2nd line therapy.
The investigators identified mRCC patients from the IMDC database who received 1st line nivolumab + ipilimumab. Available clinical and pathologic characteristics, as well as oncologic outcomes, were abstracted. Comparisons of categorical variables between patients receiving 2nd line treatments versus those that did not were performed using chi-square testing. Predictors of 2nd line therapy initiation in eligible patients were evaluated using a logistic regression model.
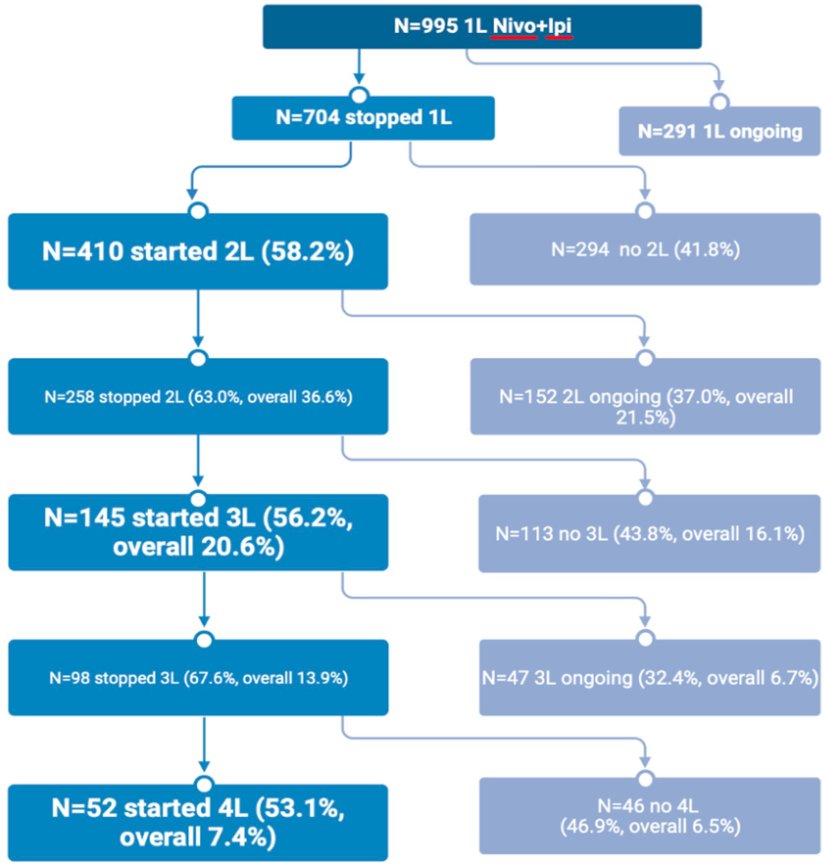
The investigators identified 995 patients, of whom 704 discontinued 1st line therapy (eligible patient cohort). Reasons for discontinuing 1st line therapy included:
- Progressive disease: 40%
- Toxicity: 25%
- Death: 4.3%
- Complete response: 1.6%
- Other reason: 29.7%
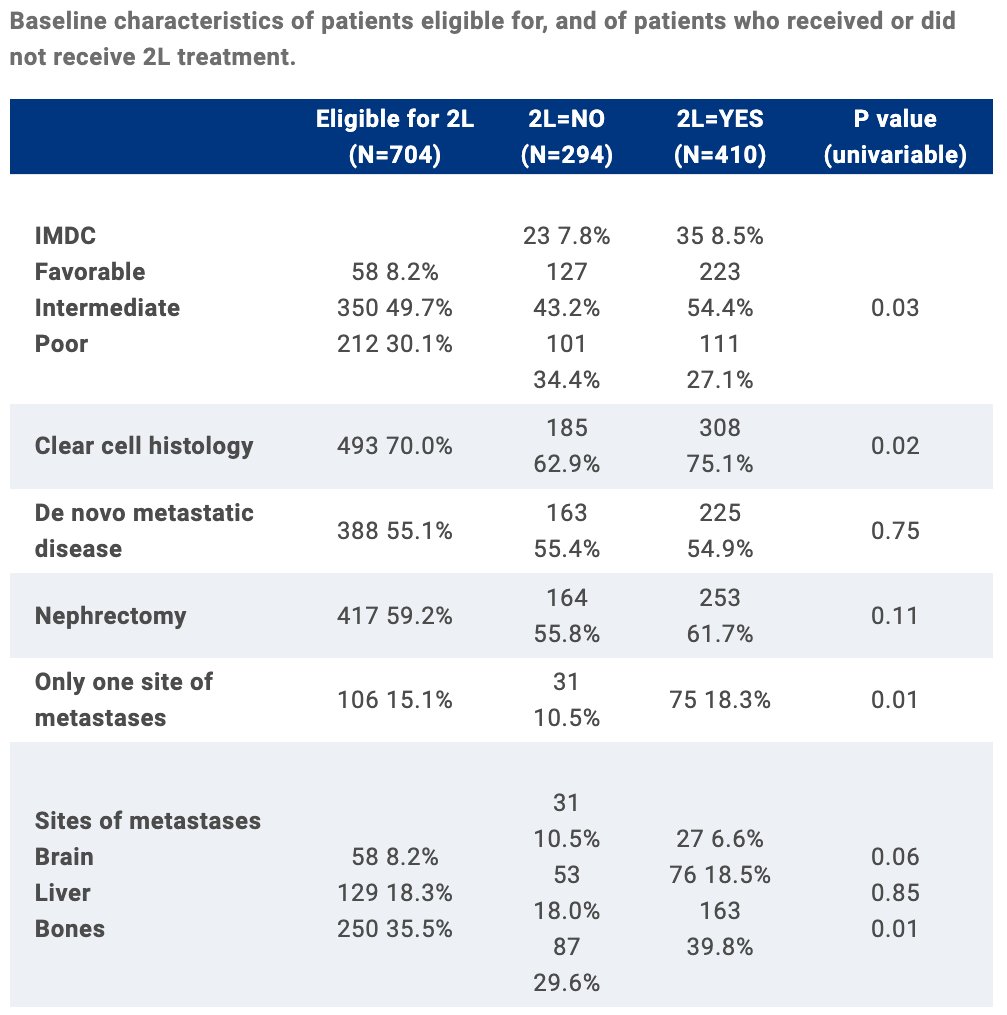
Among the 704 eligible patients, 410 (58%) received 2nd line therapy. On univariable analysis, the authors identified the following predictors of receiving 2nd line therapy:
- 1st line therapy discontinued due to progressive disease (82% received 2nd line therapy) as opposed to other reasons (43% received; p<0.001)
- Clear cell histology (75.1% of patients receiving 2nd line therapy compared to 63% of those not, p=0.02)
- Bone metastases (40% of those receiving 2nd line therapy compared to 30% of those not, p=0.01)
- One site of metastasis (18.3% of those receiving 2nd line therapy versus 10.5% of those not, p=0.01)
- IMDC poor risk status (27.1% of those receiving 2nd line therapy versus 34.4% of those not, p=0.03).
On multivariable analysis adjusting for IMDC criteria, none of the aforementioned variables were significantly predictive of the odds of receiving 2nd line therapy. Among 258 patients who discontinued 2nd line therapy, 145 (56%; overall 21%) started 3rd line therapy. Of the 98 patients who stopped 3rd line therapy, 52 (53%; overall 7.4%) started 4th line therapy.
Dr. Lemelin concluded that in this study, over half of eligible patients received subsequent lines of therapy. No predictors of 2nd line therapy initiation could be identified on multivariable analysis. Attrition rates between lines of therapy have important implications for patient counseling, cost analyses, and clinical trial design.
Presented by: Audreylie Lemelin, MD, Clinical Fellow, Tom Baker Cancer Centre, University of Calgary, Calgary, AB
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, June 2 – Tues, June 6, 2023.


