(UroToday.com) The 2023 ASCO annual meeting included a bladder cancer session, featuring a presentation by Dr. Akshay Sood discussing age, sex, and race-related differences in outcomes of patients with muscle-invasive bladder cancer (MIBC) treated with radical cystectomy. Bladder cancer is a complex and multifaceted disease, which has long been observed to exhibit substantial disparities in incidence and survival across gender, age, and racial groups. As such, it remains unclear whether the poor outcomes associated with older age, female sex, and African-American race in patients with MIBC treated with surgery are due to differential access to standard medical care or intrinsic differences in tumor biology.
Dr. Sood and colleagues designed an integrative study using two complementary datasets to answer this question. First, they used the SEER-Medicare MIBC dataset (n=2,327) to evaluate the real-world differences in survival outcomes among patients of female versus male sex, African-American versus Caucasian race, and older versus younger age before and after adjusting for demographic, tumor, treatment, and access-to-care factors. Second, they used The Cancer Genome Atlas (TCGA) project’s MIBC dataset (n=410) to evaluate the biological differences in molecular profiles of bladder tumors in these patient groups. Biological endpoints examined included DNA-level genomic alterations, mRNA expression subtypes, and RPPA-derived proteomic profiles, and clinical endpoints assessed included unadjusted and adjusted cancer-specific mortality outcomes.
Population-level analysis demonstrated that patients of the female sex (10-year cancer-specific mortality: 51.3% v 43.8%, Gray’s p<0.001), African-American race (10-year cancer-specific mortality: 56.2% v 46.1%, Gray’s p=0.022) and older age (10-year cancer-specific mortality: 47.8% >=81 y v 44.1% <=70 years, Gray’s p=0.032) had worse cancer-specific mortality at presentation:
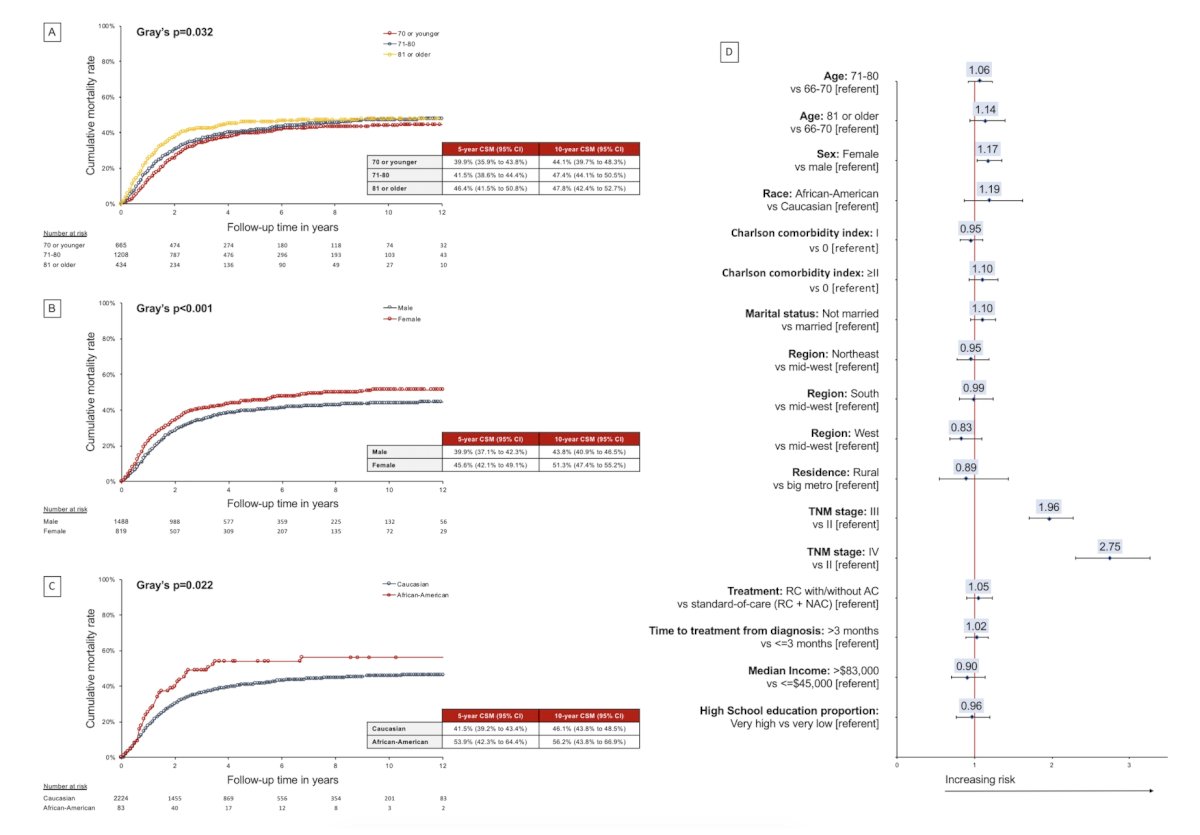
In adjusted analyses, however, only the female sex remained associated with worse cancer-specific mortality (HR 1.17, p=0.028). The TCGA analysis revealed that advanced age was associated with increased total mutational burden and neoantigen load, both of which have been associated with improved survival. No other age-related differences were seen in other DNA alterations, mRNA expression subtype distribution, or RPPA proteomic cluster profiles. Similarly, no racial differences were observed in molecular alterations at the DNA, RNA, or protein levels. However, females were noted to have adverse molecular profiles across all levels of molecular expression, including at the DNA-, RNA- and proteomic-level. Specifically, females were noted to have lower total mutational burden (in stage 3-4 cancers, median 170 versus 240, p=0.01), lower neoantigen load (in stage 3-4 cancers, median 382 versus 551, p<0.01), higher Msig2 DNA mutational signature (in stage 3-4 cancers, 65.3% versus 50.5%, p=0.04), higher basal/sq mRNA subtype (in stage 3-4 cancers, 52% versus 34.2%, p=0.02), and lower RPPA cluster1 subtype (in stage 2 cancers, 15.2% versus 36%, p<0.01):
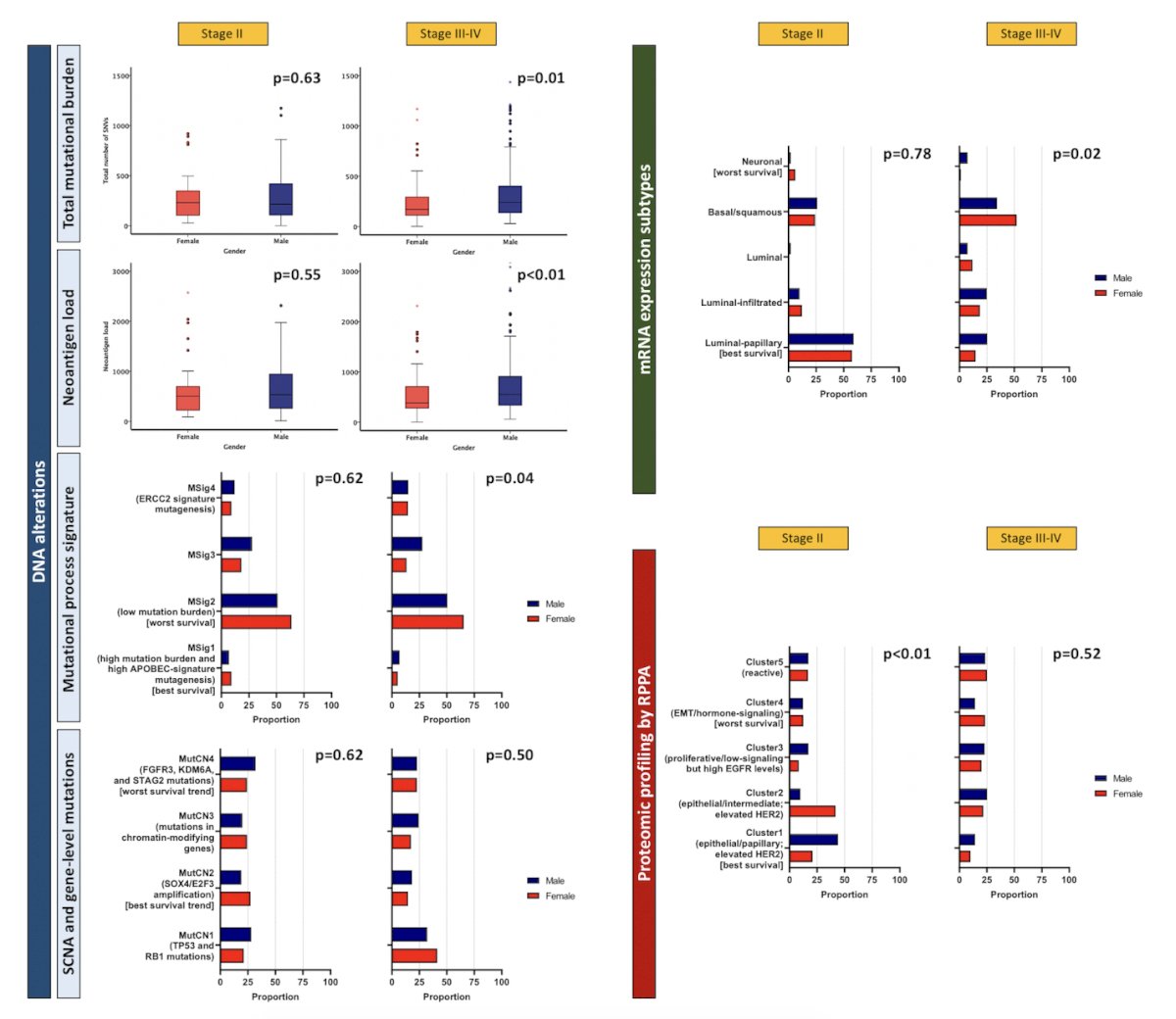
These results highlight significant biological differences among these patients, particularly when assessing by sex.
Dr. Sood concluded his presentation by discussing age, sex, and race-related differences in outcomes of patients with muscle-invasive bladder cancer treated with radical cystectomy with the following take-home messages:
- These findings suggest that the poor outcomes seen among patients of African-American race and older age in the real world are likely driven by multilevel biases in healthcare delivery, while in women they may be a result of a combination of biological and access-to-care factors
Presented by: Akshay Sood, MD, The University of Texas MD Anderson Cancer Center, Houston, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, June 2 – Tues, June 6, 2023.


