(UroToday.com) The 2022 ASCO annual meeting featured an oral abstract session on testicular cancer, including a presentation by Dr. Torgrim Tandstad discussing late relapses among testicular cancer patients. Late relapses (relapse occurring after disease-free interval of two years) in testicular cancer are relatively uncommon. The limited data published is hampered by selection bias and incomplete data regarding follow-up. Dr. Tandstad and colleagues aimed to investigate the frequency of late relapses, of very late relapses (relapse occurring after disease-free interval of five years), and of extremely late relapses (relapse occurring after disease-free interval of ten years) in a cohort treated after 1995, compared to a cohort before 1995. Finally, they aimed to describe the number of missed relapses beyond a 5-year follow-up scheme.
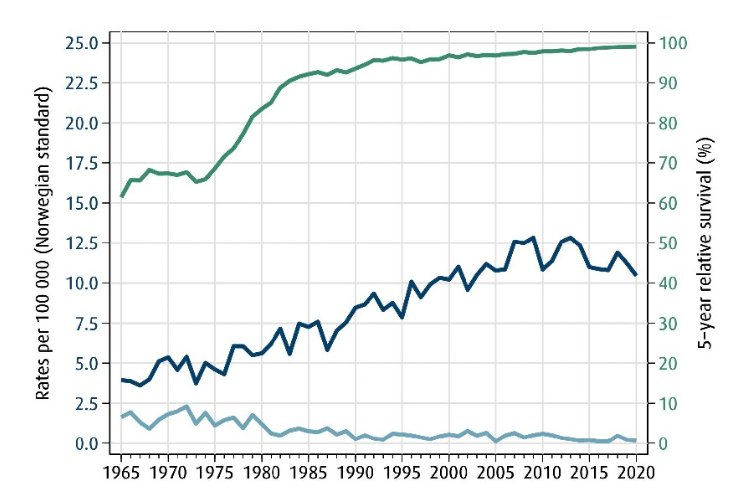
SWENOTECA was established in 1981 comprising all hospitals treating testicular cancer in Norway and Sweden. This encompasses a population of 15,500,000 and an annual testicular cancer diagnosis incidence of 600. This collaboration allowed for standardization of management programs for testicular cancer, and prospective registration of all patients with testicular cancer, with continuous evaluation of outcomes. In Norway, there has been centralization of treatment to four academic hospitals in Oslo, Bergen, Tromso, and Trondheim. As follows is a graph depicting incidence, mortality, and survival for testicular cancer in Norway:
Dr. Tandstad emphasized that there are several important research questions:
- What is the real-world rate and survival of late relapse in a complete national cohort?
- Is the current definition and use of late relapse reasonable?
- What is the impact of modern guidelines and adherence to guidelines on the prevalence of late relapse and survival?
A total of 5,712 patients, including 2,978 seminoma and 2,734 nonseminoma, were diagnosed with testicular cancer in Norway, with 2,207 patients diagnosed 1980-1994 and 3,505 patients diagnosed 1995-2009. Data are complete, due to identification by the Cancer Registry of Norway and Norwegian Cause of Death Registry. Details regarding diagnosis, stage, treatment, and follow-up were obtained from medical records. Relapse rates have been estimated using Kaplan-Meyer.
A total of 472 patients experienced relapse, including 186 seminoma and 286 nonseminoma. Of these, 109 were late relapses (51 seminomas, 58 nonseminomas), 50 very late relapses (22 seminomas, 28 nonseminomas) with 17 relapses (4 seminomas, 13 nonseminomas) beyond ten years:

The median time to late relapses was 4.7 years (range 2.0-21.6). In clinical stage I patients, there were 306 relapses (7.9%), with 1.9% late relapses, 1.0% very late relapses, and 0.5% relapse beyond ten years:
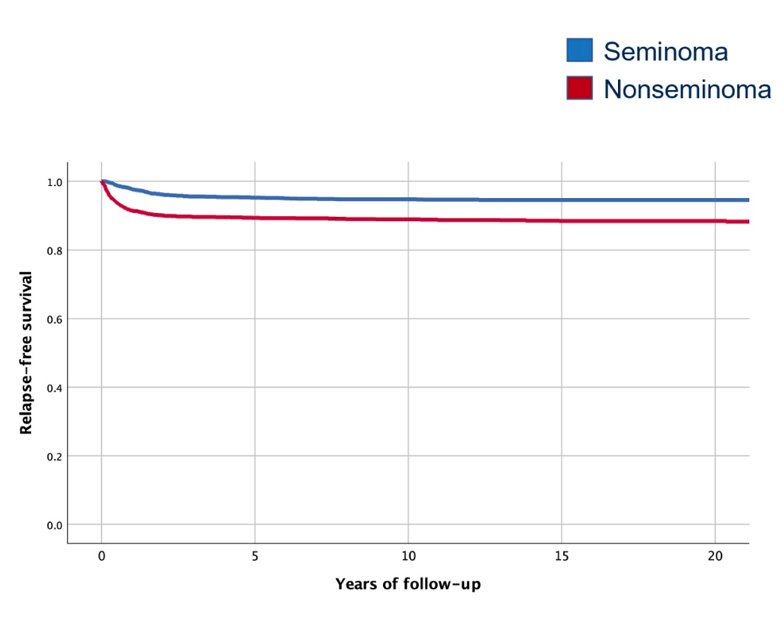
Patients followed with surveillance (n = 1,380) had a higher rate of late relapses compared to patients receiving adjuvant therapy (n = 2,619) (4.0% vs 0.9%). A total of 8 deaths occurred in 61 patients with late relapse, including 4 from testicular cancer (3 nonseminoma and 1 seminoma). In patients with metastatic disease, 166 patients experienced relapse (10.5%), with 3.6% late relapses, 1.6% very late relapses, and 0.8% relapse beyond ten years:
A total of 24 deaths occurred in 48 patients with metastatic disease with late relapse, including 17 from testicular cancer. Currently most patients with metastatic disease are treated with chemotherapy, and these patients have been reported to have the worst prognosis of late relapse. With regards to OS after late relapse among patients with metastatic disease initially treated with chemotherapy, the 10-year OS rate in the entire cohort was 49.7%. For patients diagnosed between 1980-1994, the 10-year OS rates was 34.6% compared to 60.9% for patients diagnosed between 1995-2009. Dr. Tandstad notes that these results compare favorably to those reported by Indiana University:

Outside a five-year follow-up scheme, 50 patients would be diagnosed with very late relapses. Prolonging follow-up to ten years would potentially identify only 33 of these relapses.
Dr. Tandstad concluded this presentation by discussing late relapses among testicular cancer patients with the following take-home messages:
- In this first population-based series investigating late relapses of testicular cancer with complete data regarding treatment and follow-up, there was a low rate of very late and extremely late relapses in patients treated according to modern guidelines
- Patients with CS I followed by surveillance will have higher rate of very late relapses compared to patients receiving adjuvant treatment, resulting in a higher very late relapses rate in the modern cohort, without affecting survival
- In metastatic disease, the very late relapses rate was drastically reduced in the modern cohort, with a subsequent improved survival
- The keys to improved outcomes are likely centralization of treatment, adherence to guidelines, prospective registration of patients, and subsequent reporting of results
- The broad definition of late relapse should not be used (ie. good prognosis in patients relapsing 2-5 years after treatment)
- The excellent prognosis of testicular cancer may be a potential threat to patients (becoming complacent regarding outcomes), thus centers treating testicular cancer should continuously monitor and report outcomes
Presented by: Torgrim Tandstad, MD, PhD, St. Olav's University Hospital, Trondheim, Norway
Co-Authors: Ragnhild Hellesnes, Hege Sagstuen Haugnes, Asa Karlsdottir, Carl Wilhelm Langberg, Helene F. S. Negaard, Oivind Kvammen
Affiliations: Department of Oncology, University Hospital of North Norway, Tromsoe, Norway, University Hospital of North Norway, Tromsoe, Norway, Department of Oncology, Haukeland University Hospital, Bergen, Norway, Oslo University Hospital, Oslo, Norway, Department of Oncology, Oslo University Hospital, Oslo, Norway, Department of Oncology, Ålesund Hospital, Ålesund, Norway
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, June 3 – Mon, June 7, 2022.


