(UroToday.com) Black men in the United States have higher incidence of prostate cancer and, in broad collections of data, worse outcomes. These disparities are subject to study to determine their social and biological contributors. A paucity of molecular data for Black men with prostate cancer has limited investigation to date. In fact, Black men have been under-represented in large-scale molecular prostate cancer surveys.
The PROMISE (PROstate cancer precision Medicine multi-Institutional collaborative Effort) is an expanding multi-institutional collaboration which is collecting clinical and associated molecular data on men with prostate cancer. Among the important queries being made on this valuable resource is the evaluation of any prostate cancer-related differences across self-reported racial groups with metastatic castration resistant prostate cancer (mCRPC). Biomarker selected therapies are increasingly common, molecular profiling has become standard of care. Consequently, the establishment of molecular character of mCRPCs of Black men is critical. In this analysis presented by Dr. Hwang and colleagues, all patients included had data on germline and/or somatic testing. Eligibility criteria for this analysis included a diagnosis of mCRPC with available self-reported race and biomarker data. Primary outcome was the proportion of non-Hispanic Black (NHB) and non-Hispanic White (NHW) patients with actionable molecular data. The authors defined actionability as one of the following: presence of mismatch repair deficiency or high microsatellite instability (MMRd/MSI-H), homologous recombination deficiency (HRRd), elevated tumor mutational burden (TMB ≥ 10 mut/Mb), or presence of AR-V7. Secondary outcomes included the proportion of NHB and NHW patients with molecular findings beyond those in the primary endpoint, the type and timing of genomic testing, and the use of targeted therapy.
1619 patients with mCRPC were screened with 962 meeting eligibility criteria and were included in the presented analysis. Most (78.8%) of subjects were NHW. Clinicopathological data were similar for age, PSA, distribution of metastatic sites, and receipt of prior therapies in various clinical settings (nmCSPC, mCSPC, mCRPC). Perhaps contrary to prior reports, the rates of de novo metastatic disease were similar between the two groups. Overall, NHB patients had higher initial Gleason scores (Gleason 8-10, NHB v NHB, 77.5 v 68.8%).
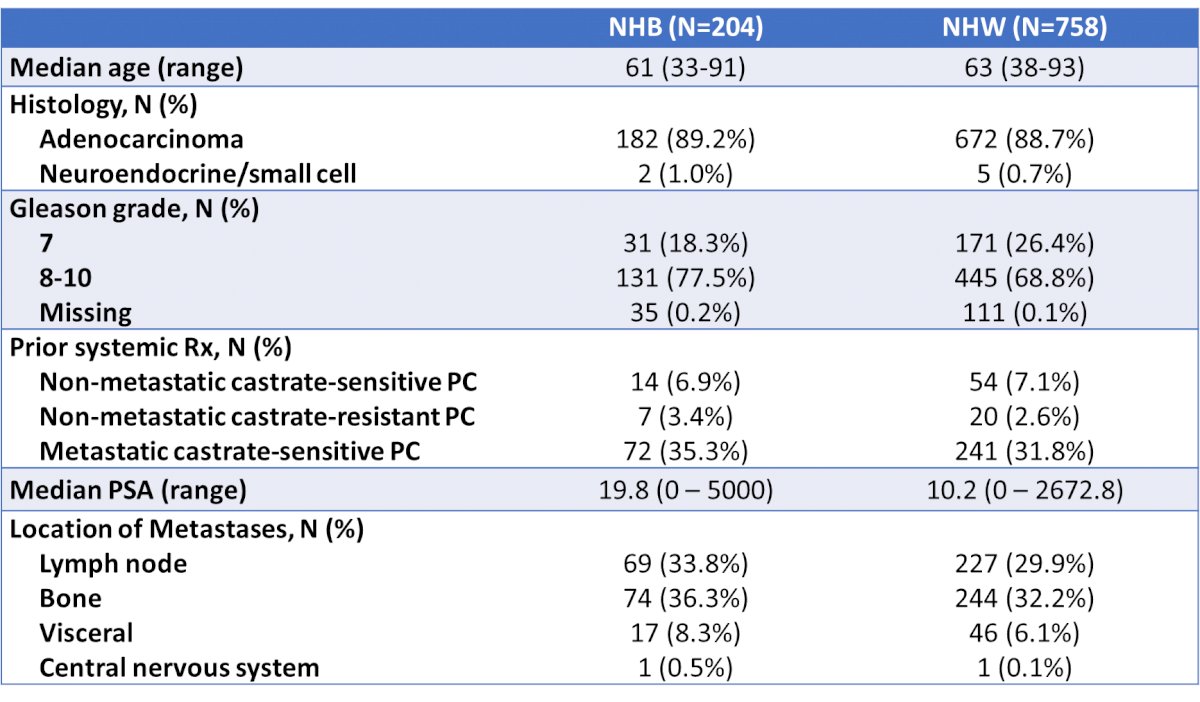
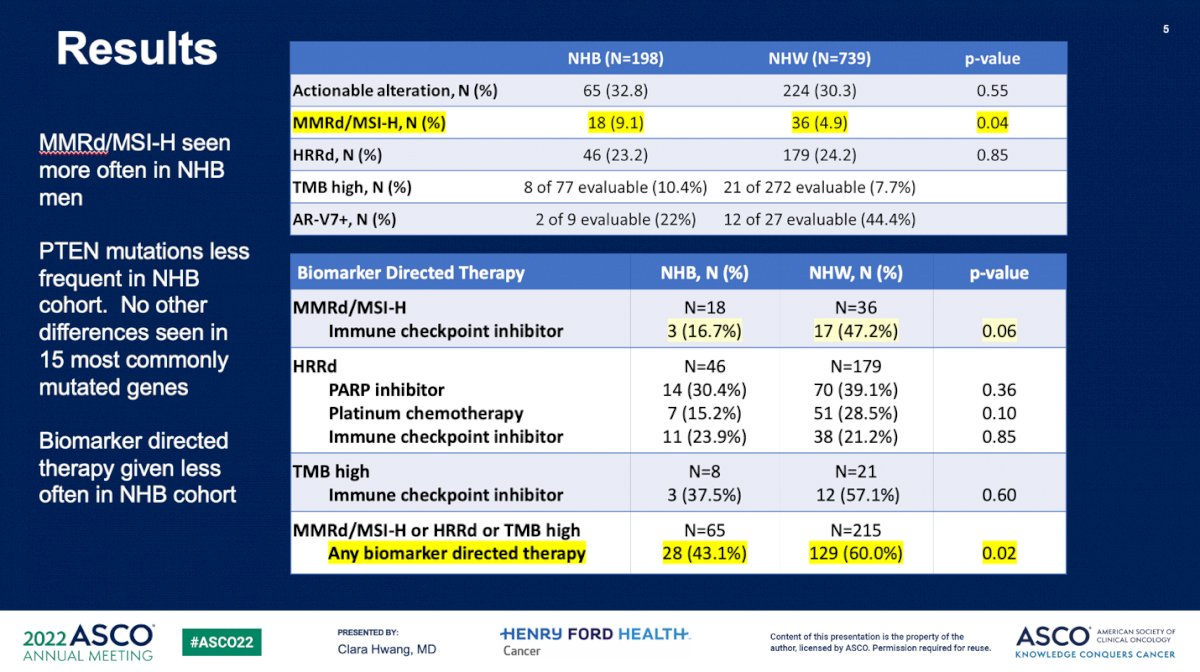
As an estimation of the use of molecular profiling, the median time from diagnosis to first molecular result was measured and found to be not different between NHB and NHW patients (56.3 v 58.7 months, p = 0.45). Blood- , rather than tissue-based, molecular testing was more common in NHB (48.7% v 36.4%, p < 0.001). The rate of any actionable alteration was similar between the two groups (NHB 32.8% v NHW 30.3%). When molecular alterations were evaluated separately, MMRd/MSI-H was found to be more common in NHB men (9.1% v 4.9%, p = 0.04), yet not different in the other molecular classification classes.
Frequency of relevant alteration in fifteen common prostate cancer genes were also compared. These genes included AR, PTEN, MYC, FOXA1, TMPRSS2, and SPOP. The “aggressive-variant”-defining (AVPC) alterations of PTEN, TP53, and RB1 were also analyzed together. Only the frequency of PTEN alterations was found to be different between groups, with NHB less likely to harbor an alteration (NHB 12.7% v NHW 23.8%, p = 0.0001). A statistically-significant de-enrichment in PTEN mutations matches previously published data. The AVPC group frequency was not different (13.1% v 18.%, p=0.13).
For molecular testing to influence patient care, the results must be interpreted and used in treatment decision-making. As a proxy for this, Hwang et al. matched treatments to molecular alterations. Overall, no difference was observed in frequency of testing-targeted therapy. For those patients with MMRd/MSI-H, rates of immune checkpoint inhibitor (ICI) use were measured. Despite a higher rate of MMRd/MSI-H, there was a trend toward less frequent use of ICI in NHB men when limited to those with the biomarker (16.7% v NHW 47.2%, p = 0.06). When taken together in sum (MMRd/MSI-H or HRRd or TMB high), NHB patients were less likely to receive any biomarker-directed therapy tailored to their molecular status (43.1% v 60.0%, p = 0.02).
Median overall survival following diagnosis of mCRPC was not different between groups for NHB and NHW men, respectively (41.5 mo, 95% CI 34.7-51 vs 44.7 mo, 95% CI 41.1-51.5; p=0.14).
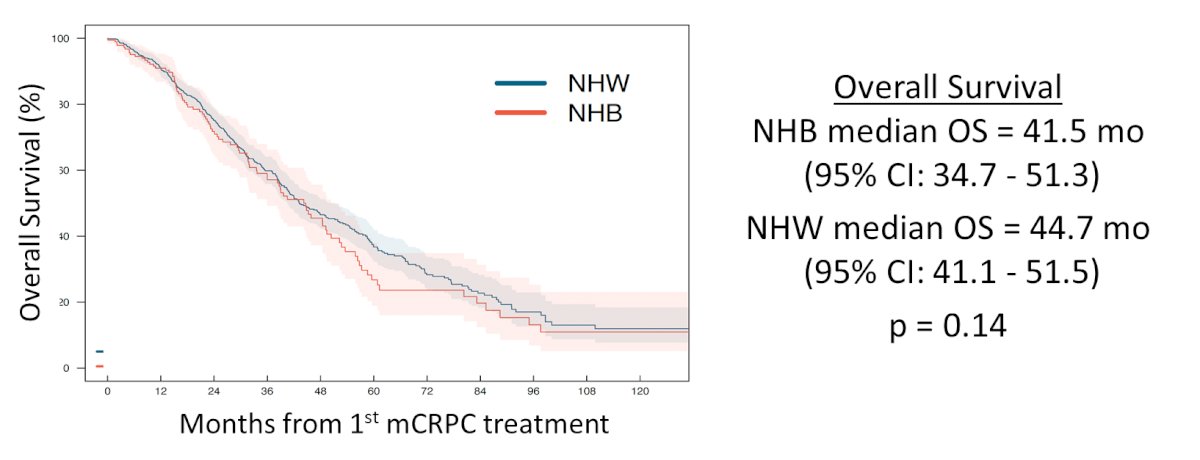
Dr. Huang conclusions highlighted their detection of more frequent occurrence in NHB patients of MMRd/MSI-H and lesser frequency of PTEN alterations. The application of genomic data for tailoring of treatment appeared to be less commonly done for NHB patients versus their NHW counterparts. Future directions included a larger dataset and also extended analysis of outcomes to molecularly-tailored therapies.
These data represent the suggestion of possible genomic differences between NHW and NHB patients with prostate cancer and demonstration of the insufficiently successful deployment of precision oncology in non-White patient groups. Classification of ancestry rather than self-reported race may refine these data, as well as expansion into broader hypothesis-generating genomic assessments.
Presented by: Clara Hwang, MD, Henry Ford Health System, Detroit, MIWritten by: Jones Nauseef, MD, PhD, Assistant Professor of Medicine within the Division of Hematology and Medical Oncology, Sandra and Edward Meyer Cancer Center, and Englander Institute for Precision Medicine Weill Cornell Medicine and Assistant Attending physician at NewYork-Presbyterian Hospital. @DrJonesNauseef on Twitter during the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, June 3 – Mon, June 7, 2022.


