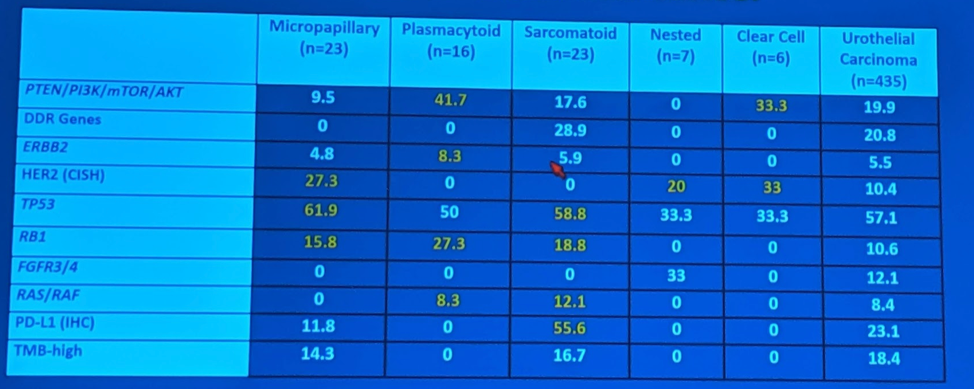
Ramamurthy et al. completed a genomic analysis of variants and found the following genes to be upregulated1:
Urothelial Carcinoma with Squamous Differentiation:
This is the most common variant, occurring in 20-30% of urothelial carcinomas of the bladder.
Extensive squamous differentiation (>50%) is associated with higher grade tumors and shorter disease-free periods; also associated with decreased cancer-specific survival.
However, she notes that neoadjuvant chemotherapy can still be effective in patients with variant histology. Interestingly, looking retrospectively at some of the large neoadjuvant chemotherapy (NAC) trials, including SWOG 8710, variant histology patients actually had a higher rate of pT0 downstaging, as seen below:
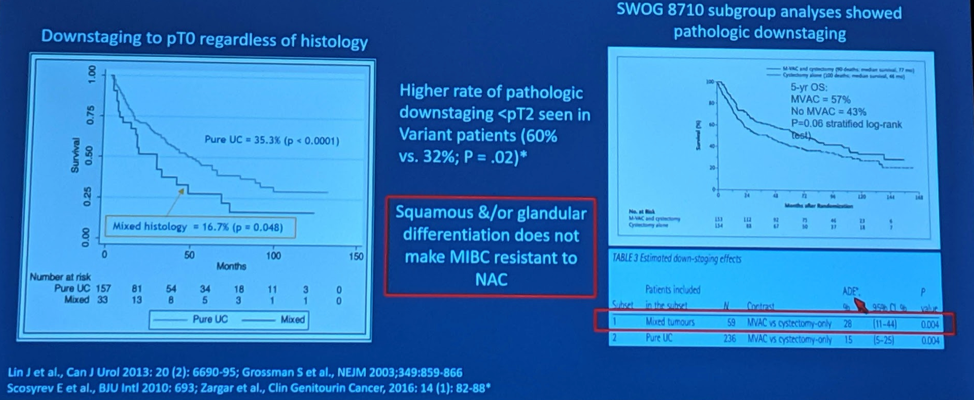
So, NAC should not be held in this setting.
Briefly, Dr. Aragon-Ching also addressed trimodality therapy (TMT), which is maximal TURBT followed by chemoradiation. Data by Krasnow et al., highlighting the Boston TMT experience, demonstrated no difference in disease-specific and overall survival in the 22% of patients with variant histology.2
Plasmacytoid Variant:
This is a rare variant, and so much data is not available. However, the 2 largest series of 31 patients (MD Anderson) and 98 patients (MSKCC) indicate that this is a very aggressive variant. Median overall survival was 17.7 months, but it was stage dependent (45.8 months for stage 1 vs. 13.3 months for stage 3-4). Upstaging and positive margins are common in these patients.
They did still note 80% pathologic downstaging with NAC, however, so it should still be considered.
Unique to this histology is the nearly 80% peritoneal recurrence rate. This may be due to the high expression of CDH1 which results in loss of E-cadherin expression. May result in enhanced cellular migration.
Micropapillary Variant:
This is seen in 0.6-1% of urothelial carcinomas and was first described in 1994. It is predominantly in male patients (5-10: 1). With regards to NAC, a systematic review by Abufarai et al. confirmed that NAC is NOT effective for the micropapillary variant.3 While downstaging to ypT0 is seen in 11-55% of patients, it was not associated with relapse-free survival (RFS), disease-specific survival (DSS) or overall survival (OS). Hence, early upfront radical cystectomy is recommended for patients with T1 disease.
Unfortunately, guideline recommendations for variant histology appear vague.
- AUA: Consider unique clinical characteristics that may require a divergence from standard evaluation and management (expert opinion)
- EAU: Variant histology should be considered a highest-risk tumor
- NCCN: Micropapillary, plasmacytoid and sarcomatoid variant histology are generally at higher risk of progression for MIBC and a more aggressive approach should be considered.
Presented by: Jeanny B. Aragon-Ching, MD, FASP, Clinical Program Director of Genitourinary Cancers, INOVA Schar Cancer Institute, Fairfax, VA
Written by: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University, @tchandra_uromd, @JEFFUrology at the 2019 ASCO Annual Meeting #ASCO19, May 31- June 4, 2019, Chicago, IL USA
References:
Written by: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University, @tchandra_uromd, @JEFFUrology at the 2019 ASCO Annual Meeting #ASCO19, May 31- June 4, 2019, Chicago, IL USA
References:
- Ramamurthy et al. GU ASCO 2019.
- Krasnow et al. EU 2017.
- Abufarai et al. EU 2019.


