(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) meeting featured a session on the identification, assessment, and management of side effects of systemic therapies, and a presentation by Dr. Lisa Horvath discussing how to assess and treat gynecomastia.
Dr. Horvath emphasized that it is important to distinguish at the time of diagnosis the difference between gynecomastia versus chest fat. Gynecomastia features include (i) enlargement of breast tissue (nodular mass), (ii) enlargement of nipple and areola size, and (iii) tenderness/sensitivity. Chest fat features include no palpable mass in the breast tissue and normal nipple/areola size. Radiology to assess subareolar changes can be accomplished with a breast ultrasound or mammogram. The pathophysiology of gynecomastia is as follows:
Dr. Horvath highlighted that the baseline rate of gynecomastia with ADT +/- ARPI is 7-9% and summarized in the table stratified by treatment agent and clinical trial: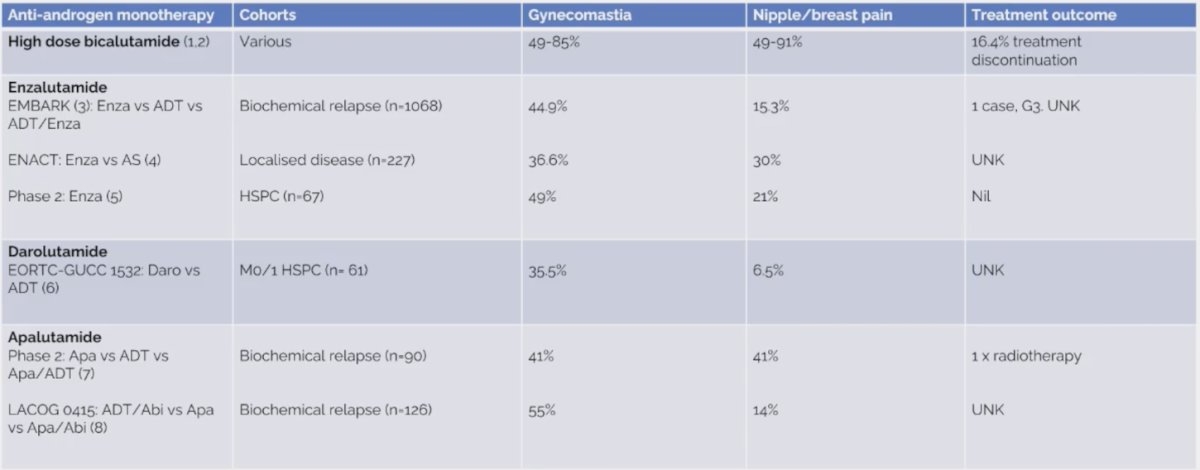
Studies assessing the impact of prophylactic radiotherapy included studies enrolling patients treated with bicalutamide 150 mg PO daily, with radiotherapy given prophylactically on the day hormonal treatment started: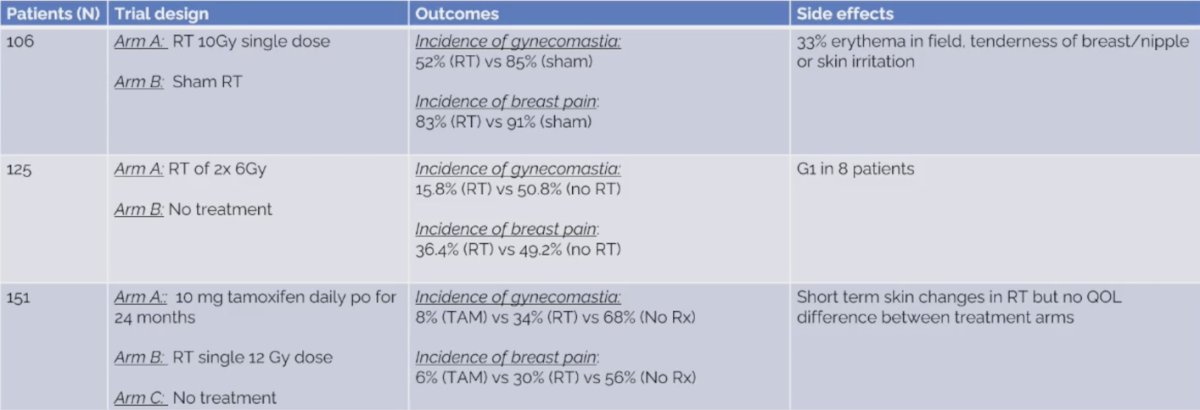
Studies assessing the impact of prophylactic systemic treatment included studies enrolling patients treated with bicalutamide 150 mg PO daily, with systemic therapy given prophylactically on the day hormonal treatment started: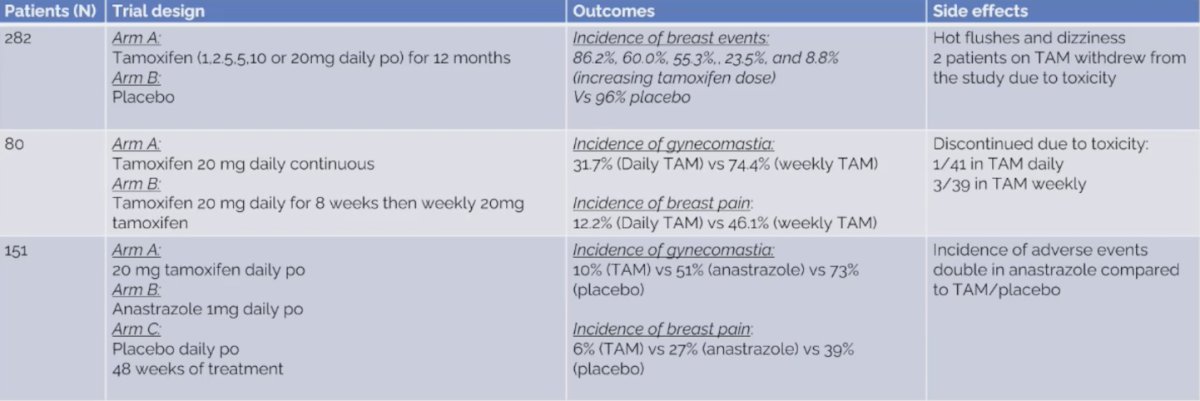
Viani and colleagues previously performed a systematic review assessing tamoxifen or radiotherapy for prevention of gynecomastia and breast pain.1 Among six randomized clinical trials (n = 777), there was a significant reduction in the incidence of gynecomastia and breast pain rates in patients treated with radiotherapy (OR 0.21, 95% CI 0.12–0.37, p < 0.0001; OR 0.34, 95% CI 0.20–0.57, p < 0.0001, respectively). Use of radiotherapy resulted in a number needed to treat of 3.4 and 5 to avoid one case of gynecomastia and breast pain, respectively. Pooled results from trials comparing tamoxifen versus observation showed a statistical benefit for breast pain and gynecomastia in favor of tamoxifen arms (OR 0.04, 95% CI 0.02–0.08, p < 0.0001; OR 0.07, 95% CI 0.0–0.14, p < 0.00001). Tamoxifen resulted in a number needed to treat of 1.56 and 2.1 to avoid one case of gynecomastia and breast pain, respectively.
With regards to drug-drug interactions, enzalutamide and apalutamide may decrease the level or effects of tamoxifen by affecting the hepatic/intestinal enzyme CYP3A4 metabolism. Thus, do we need a higher dose than 20 mg tamoxifen? For darolutamide, there was no interaction.
The role of surgery is for symptomatic gynecomastia. Options include minimally invasive options (liposuction, vacuum-assisted mastectomy), skin-sparing mastectomy, and mastectomy with skin reduction. Complication rates from surgery are ~5.8% incidence of hematoma and ~2.4% incidence of seroma.
Dr. Horvath notes that there are several questions for the future:
- Will tamoxifen work as well with enzalutamide, apalutamide, and darolutamide?
- Does the tamoxifen need to be adjusted for enzalutamide and apalutamide?
- Can patients tolerate tamoxifen + ARPI combination beyond 12 months?
- The role of radiotherapy or surgery, are these one-off treatments for long-term ARPI therapy?
- What is the patient perspective on treatment options?
Dr. Horvath concluded her presentation discussing how to assess and treat gynecomastia with the following take-home messages:
- Gynecomastia is prevalent in ARPI monotherapy
- Tamoxifen is a better prophylactic treatment than radiotherapy
- Prophylactic tamoxifen is better than treating at diagnosis of gynecomastia
- Surgery should be reserved for symptomatic gynecomastia
Presented by: Professor Lisa G. Horvath, MBBS, PhD, University of Sydney, Sydney, New South Wales, Australia
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference, Lugano, Switzerland, April 25th - April 27th, 2024
References:
- Viani GA, Da Silva LGB, Stefano EJ. Prevention of gynecomastia and breast pain causes by androgen deprivation therapy in prostate cancer: Tamoxifen or radiotherapy? Int J Radiat Oncol Biol Phys. 2012 Jul 15;83(4):e519-524.


