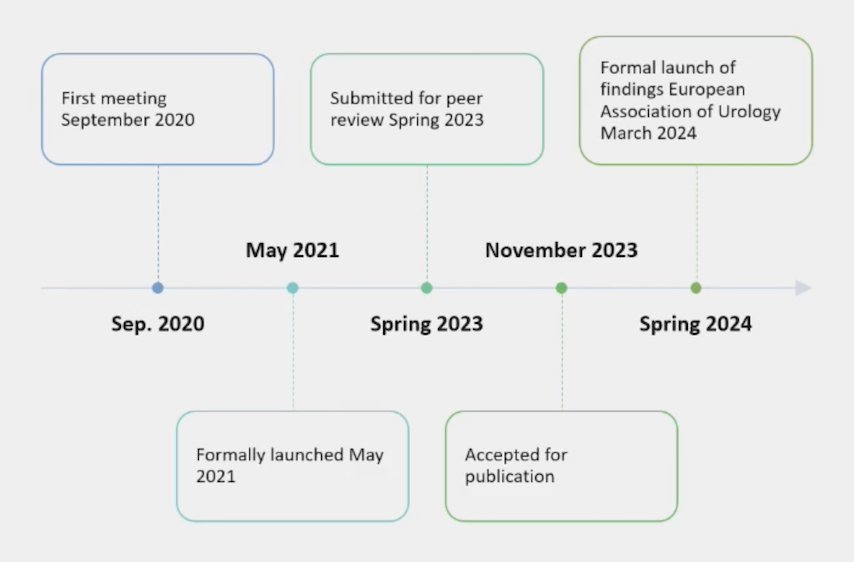
(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) meeting featured a session on global access to advanced prostate cancer in low- and lower-middle-income countries, and a presentation by Dr. Nicholas James discussing the Lancet Commission on Prostate Cancer and the forthcoming surge in prostate cancer. Dr. James notes that the first meeting of the Lancet Commission on Prostate Cancer took place in September 2020, followed by a formal launch in May 2021, submission of the paper for peer review in Spring 2023, accepted for publication in November 2023,1 and formal launch of findings at the European Association of Urology in March 2024:
The Lancet Commission on Prostate Cancer has the following chairs and topics:
- Ian Tannock: Improving the evidence base in low- and middle-income countries
- James N’Dow: Reducing the risk of overdiagnosis while increasing diagnosis of curable disease
- Felix Feng: Better management of early disease
- Silke Gillessen: Optimizing treatment of advanced disease
Dr. James notes that prostate cancer is the most common male cancer in 112/185 countries and makes up 15% of all male cancers. Importantly, cases will rise from 1.4 million per year to approximately 3 million in 2040: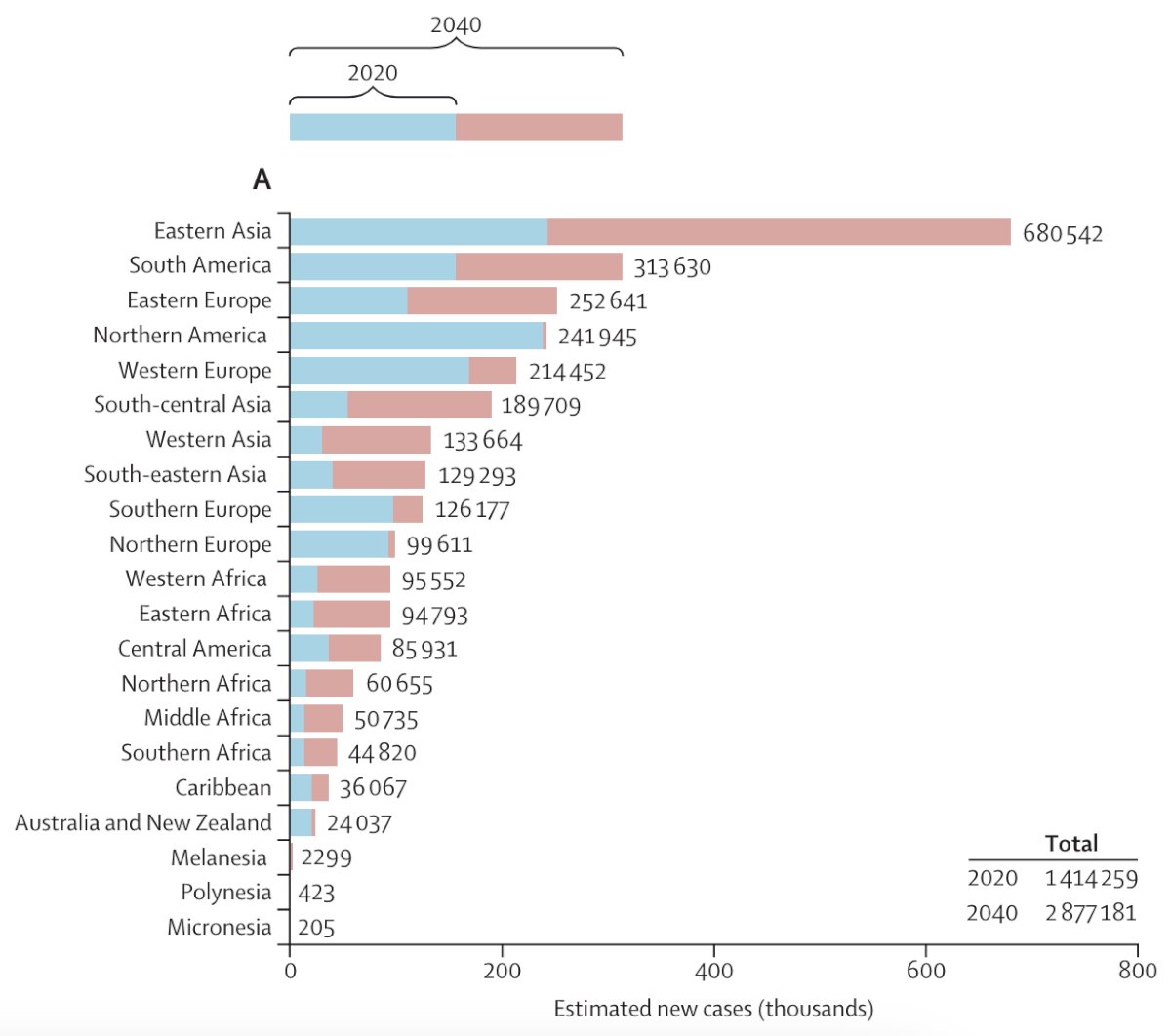
Mortality is also set to rise sharply in low- and middle-income countries: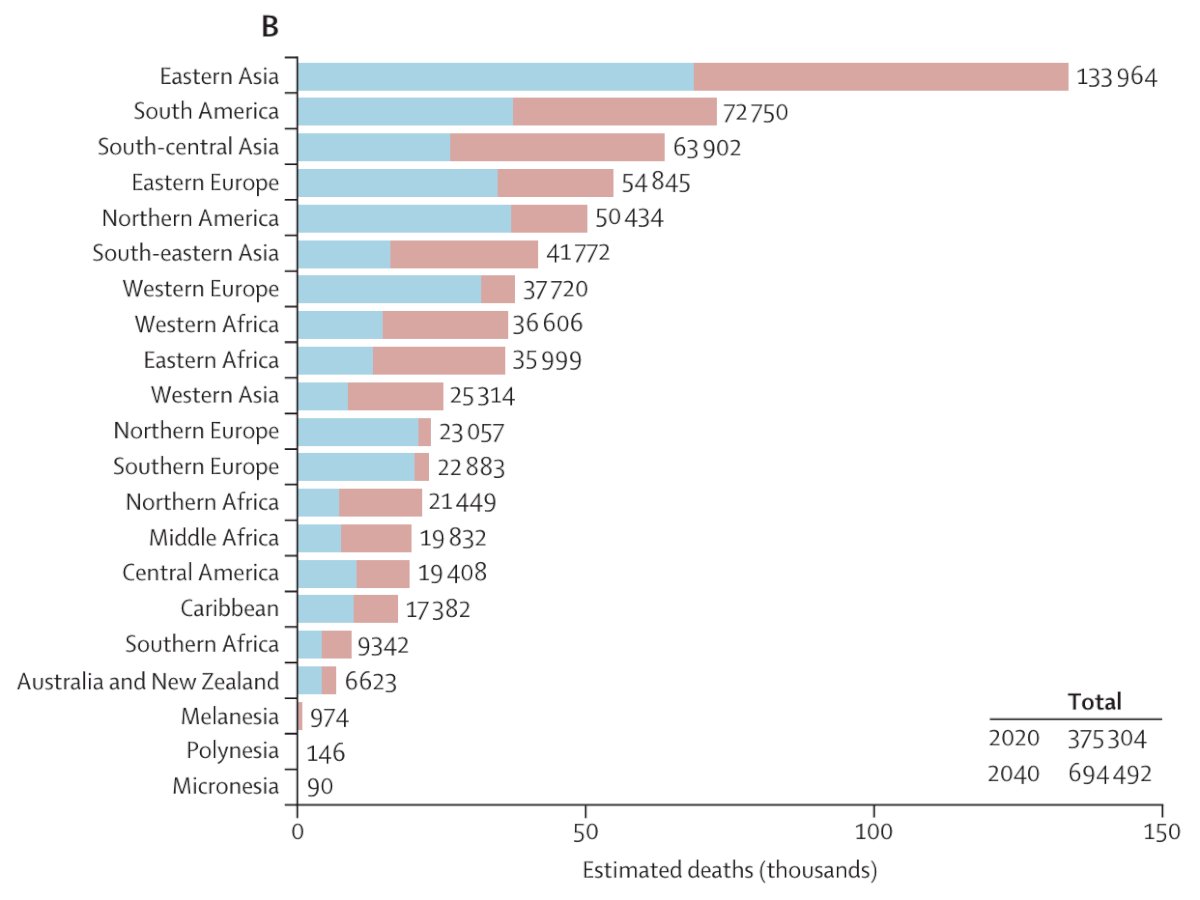
Dr. James notes that metastatic disease is incurable, therefore, to reduce deaths we must diagnose before disease spreads. In high-income countries, a significant minority of men still present with advanced disease. However, in low- and middle-income settings, the majority of men present with advanced disease. With rapidly rising cases, this will present an increasing problem. As such, early diagnosis systems will need to incorporate novel skill mixes. Integration of artificial intelligence to aid interpretation of scans and biopsy samples will be important. The rise in prostate cancer will be mirrored by other conditions such as diabetes and heart disease, so a broader focus is desirable. Outreach programs are needed that harness new communication channels, such as smartphones.
With regards to ethnicity, in high-income countries, prostate cancer is twice as common in men of African origin. However, globally, ethnic origin is a key driver of high death rates. Incidence rates globally are driven by a mix of rates of PSA testing and underlying prevalence, and high death rates are driven by stage at diagnosis and rates of disease. Treatment of advanced prostate cancer remains a problem, and affordable therapies are available but are unevenly distributed. Consistent use of available therapies is a cost-effective way to reduce harm from prostate cancer. Moreover, there remains a shortage of specialist surgeons and radiotherapy equipment in low- and middle-income countries, and addressing this shortage is key to improving prostate cancer care globally.
Dr. James then discussed four action items:
- Action 1: Improve diagnostic pathways in all healthcare settings to facilitate early detection of clinically significant prostate cancer and integrate with a broader focus on men’s health issues
- In high-income settings: incorporation of pre-biopsy MRI scanning in at least 50% of cases with suspected prostate cancer to reduce overdiagnosis of low-grade disease
- In low- and middle-income settings:
- Establishment of outreach services offering information, PSA testing, and onward referral for diagnosis and treatment
- More than 50% of men are diagnosed in low- and middle-income countries with advanced disease leading to an overall death rate in Africa of over 60%
- If the proportion diagnosed late were reduced to 1 in 3, this death rate would be halved
- Action 2: Create cloud-based medical record systems to improve access to health information and to facilitate the use of artificial intelligence to complement or supplement deficits in health profession numbers and skills
- Access to, and control of, medical information allows tailored advice and assistance with the navigation of medical systems
- Leveraging the broad availability of smartphones globally and linkage to the extensive online information resources could transform how people in low- and middle-income countries access healthcare
- In high-income countries, smartphone health apps are increasingly popular. Their use should be strongly supported to give more control to patients have over their healthcare
- Action 3: Implement pragmatic practice recommendations for maximum benefit, tailored to national resource levels and patterns of disease
- Guidelines should be resource-appropriate and linked to patient-held record systems
- At present, in high-income countries with funded health care, evidence shows low levels of compliance with guidelines. Consistently delivering what is known to work can rapidly improve outcomes
- In high-income countries, 80% of men with metastatic disease should receive combination androgen deprivation therapy
- In low- and middle-income countries, orchiectomy should be offered instead of GnRH agonists either at diagnosis or once treatment is established
- Savings can be used to pay for additional therapies, such as generic low-dose abiraterone
- Action 4: Support research on risk-stratified regulatory models, and on better understanding of the effects of ethnic differences
- Research on cost-effective diagnostic methods and drug repurposing or dose de-escalation
- In low- and middle-income countries, at least one trial each of screening, early diagnosis, and treatment should be established within the next five years
- Trials should reflect the ethnic mix of the study population. In international trials, broad geographical spread is a route to better ethical representation
- Ethnic representation in licensing trials should be measured and mandated by regulatory bodies
- Under-representation in studies of men of African origin is a particular, but not the only, concern
Dr. James concluded his presentation discussing the Lancet Commission on prostate cancer and the forthcoming surge in prostate cancer with the following take-home messages:
- We need to improve diagnosis and integrate prostate cancer with men’s health
- We need to empower patients with informed care
- We need to implement resource-sensitive guidelines for treatment
- Improve research and evidence-based practice and policy
Presented by: Professor Nicholas D. James, MBBS, PhD, The Institute of Cancer Research, London, UK
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference (APCCC) Meeting, Lugano, Switzerland, Thurs, Apr 25 - Sat, Apr 27, 2024.
References:


